Rheumatoid Arthritis Versus Osteoarthritis: What’s the Difference?
Learn how the symptoms, diagnosis and treatment for RA and OA differ — and why this information can help you work together with your doctor to get the best care.
Rheumatoid arthritis (RA) and osteoarthritis (OA) can both cause considerable pain and joint problems, but they are two of the many different types of arthritis. What is the difference between the two conditions?
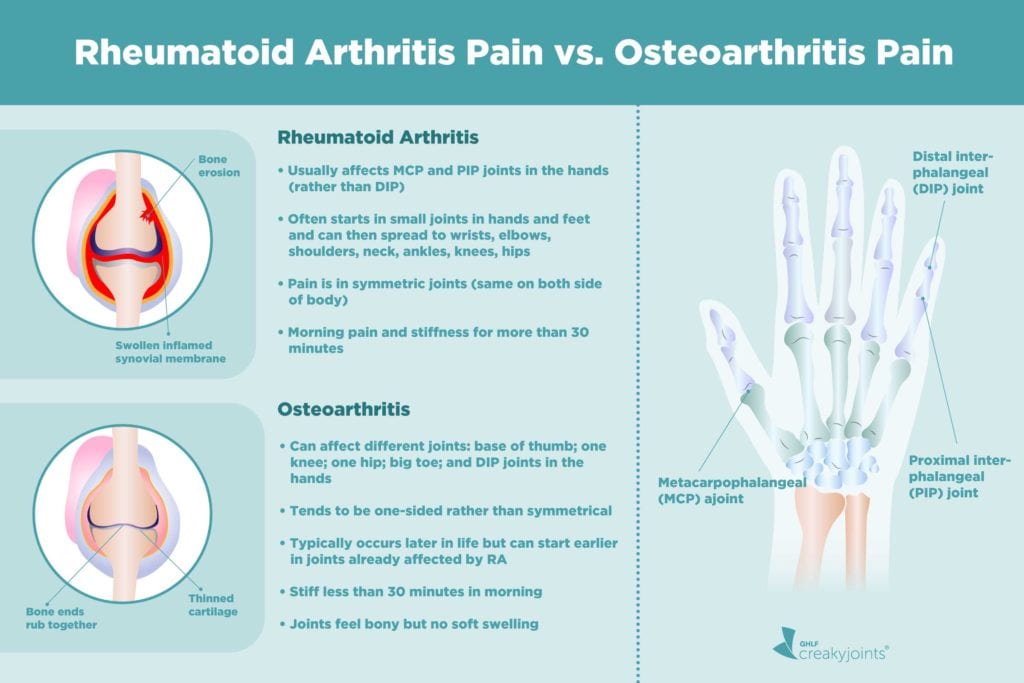
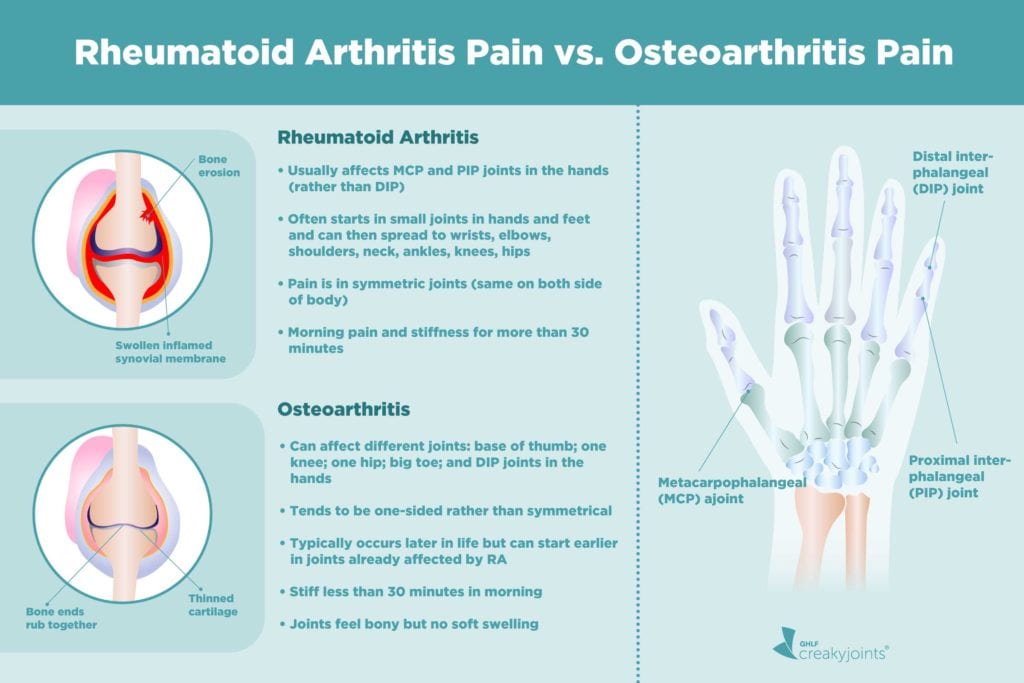
RA is an autoimmune disease that occurs when the immune system malfunctions and starts attacking healthy tissues, mainly the synovium (the linings of joints). The same inflammation affecting the joints can also damage organs, including your eyes, skin, heart and lungs.
Unlike RA, OA is not an autoimmune disease. You get it when articular cartilage — the smooth, white tissue at the ends of bones where they meet to form joints — breaks down. This breakdown is the result of daily wear and tear.
“As I like to tell my patients, OA is a type of wear and tear arthritis, similar to a tire wearing down with use, whereas RA is an autoimmune disease where you try to fix the problem as closely as possible,” says Dr Jiha Lee, a rheumatologist at the University of Michigan Health.
These are the main differences between RA and OA. But many more differences can help your doctor determine what type of arthritis you have and your treatment options.
More Differences
According to a 2020 report in Preventive Medicine Reports, OA affects more than 30 million US adults, making it one of the most common arthritic conditions. On the other hand, RA is the most common systemic (whole-body) autoimmune disease affecting about 0.5 per cent to 1.0 per cent of the American population.
Both RA and OA cause inflammation of joints, but with RA, there is much more inflammation. In recent years, researchers have found inflammation can occur in OA leading to radiographic and pain progression but are unsure of the role of inflammation and whether it is the cause of OA or the result.
OA and RA can share some symptoms, but RA often affects multiple joints in a symmetrical (on both sides of the body) fashion. OA will affect only a few joints in various places aroun the body. RA also causes flu-like symptoms, such as fever and malaise (a general unwell feeling).
Which Is Worse — RA or OA?
The progression of RA is more challenging to predict. OA tends to be more predictable as symptoms are limited to affected joints. Nonetheless, OA can still be a debilitating condition.
“Both conditions cause a lot of disability and loss of function. In the case of RA, we have treatments that can slow down the disease process and achieve remission. With OA, there is a progression over time,” says Dr Lee. Either condition can potentially lead to surgery down the road.
Remission in RA generally refers to a period of no symptoms or very few symptoms.
RA versus OA: Getting a Correct Diagnosis
The treatment goals for both RA and OA are similar — to maintain joint function, reduce pain and minimise the potential for joint damage. But these conditions need to be treated and managed differently, which makes getting the correct diagnosis crucial.
With RA, diagnosis involves a medical history, physical examination, bloodwork and imaging studies. Your medical history in RA is helpful because there is a genetic component to the disease.
An OA diagnosis typically involves a medical history, physical examination and imaging studies. Bloodwork might be done to rule out RA and other types of autoimmune arthritis.
With this overlap in diagnosis, RA is sometimes mistaken for OA — “It often happens, especially as patients get older,” Dr Lee says. This is especially common in erosive OA. It can be mistaken at times, leading to delays in diagnosis and treatment.” Erosive OA is a rarer, more severe type of OA involving bone erosion and cartilage damage to the fingers.
The Role of Imaging
According to Dr Lee, X-rays, ultrasound scans and magnetic resonance imaging (MRI) can help distinguish RA from OA. “They do have different patterns in terms of the joint damage that occurs.”
Dr Lee adds that X-rays can be less reliable early on. “Changes on X-rays take time to show up. Ultrasound and MRI can show inflammation better and point you more to OA versus RA.”
The different types of imaging can reveal distinct patterns of arthritic damage in both RA and OA. For example, X-rays can show cartilage loss, bone spurs and other bone damage. MRI and ultrasound can offer more detailed images of soft tissues like tendons and ligaments, cartilage and the synovial lining of joints.
With OA, imaging can reveal joint damage in the weight-bearing joints, mainly the knees and hips. “With that, you will see joint space narrowing between the bones at the joints where cartilage has worn away,” says Dr Lee.
When that joint space narrowing occurs, the cartilage can no longer keep bones apart, and bones start to painfully rub against each other.
On imaging, RA is distinguishable from OA because, according to Dr Lee, “RA, especially in the hands and feet, leads to erosive changes at the bone.”
Bone erosion means there is a loss of bone or bone destruction.
Can RA and OA Co-Exist?
It is possible to have both RA and OA. OA is more likely to occur as you age, and people with RA are at risk for OA as they get older. It is also possible to have elderly-onset RA years after being diagnosed with OA.
According to a 2018 report in the journal Therapeutic Advances in Musculoskeletal Disease, elderly onset RA, or geriatric RA, begins after age 65. It presents with more systemic symptoms (fever, malaise, etc.) and more frequently affects large joints (knees and the hips) rather than the small joints of the hands and feet.
When these conditions co-exist, diagnosing and treating both conditions can be challenging. “Both patients and doctors have difficulty differentiating between pain caused by either condition, says Dr Lee. “That can lead to function and mobility problems and delayed treatment.”
Getting Prompt Treatment for RA and OA
If you have experienced signs of RA or OA, you will want to see your doctor as soon as possible. If RA diagnosis and treatment are delayed, severe joint damage can occur. Delays in an OA diagnosis and treatment could mean increased pain and stiffness and a loss of mobility.
Fortunately, there are plenty of treatment options for both RA and OA, and some, such as nonsteroidal anti-inflammatory drugs, analgesics (painkillers), and prescription pain relievers can treat both. Immunosuppressive therapies, including methotrexate and biologics, can slow down the effects of the immune system and reduce inflammation. RA and OA are also managed by following a healthy lifestyle, including exercise, weight loss, proper nutrition, and stress management.
This information should never replace the information and advice from your treating doctors. It is meant to inform the discussion that you have with healthcare professionals, as well as others who play a role in your care and well-being.
This page content has been adapted, with permission, from a corresponding article by Lana Barhum on the CreakyJoints US website. Some content may have been changed to suit our Australian audience.
Keep Reading
A Patient’s Guide to Living with Rheumatoid Arthritis in Australia
Sources
Mohammed, A., Alshamarri, T., Adeyeye, T., Lazariu, V., McNutt, L., & Carpenter, D. O. (2020). A comparison of risk factors for osteo- and rheumatoid arthritis using NHANES data. Preventive Medicine Reports, 20, 101242. https://doi.org/10.1016/j.pmedr.2020.101242
Sanchez-Lopez, E., Coras, R., Torres, A. et al. Synovial inflammation in osteoarthritis progression. Nat Rev Rheumatol 18, 258–275 (2022). https://doi.org/10.1038/s41584-022-00749-9
Kobak, S., & Bes, C. (2017). An autumn tale: geriatric rheumatoid arthritis. Therapeutic Advances in Musculoskeletal Disease. https://doi.org/10.1177/1759720X17740075





