Ankylosing Spondylitis Versus Sciatica: What’s the Difference?
Ankylosing spondylitis (AS) and sciatica are painful back conditions that have different causes and treatments. We’ve shared how to tell them apart and find the right care.
Back pain of any kind can be frustrating and debilitating but figuring out what’s causing the pain can be tricky. Part of the challenge is that some back-related conditions share common symptoms.
There are many types of back pain and they differ in their cause and treatment. If you experience back pain, it’s important to have it diagnosed and treated back pain by a doctor as soon as possible to avoid unnecessary pain, disability and other complications.
Two conditions that can have overlapping symptoms are ankylosing spondylitis (AS) and sciatica. We’ve outlined how these conditions differ in their cause, symptoms and treatment.
Understanding Ankylosing Spondylitis
Ankylosing spondylitis is a form of autoimmune arthritis that falls under the umbrella of axial spondyloarthritis (axSpA) and is associated with persistent lower back pain.
In autoimmune conditions, the normal signals that tell your immune system to protect your body from harm by viruses, bacteria or injuries, overreact. In AS, this usually causes inflammation, pain and stiffness in the spine and the sacroiliac (SI) joints located just above the tailbone.
AS can cause bony growths on the spine. Over time, these growths can cause parts of the spine to fuse, which limits mobility. It is a chronic (ongoing) condition and symptoms can come and go but it is not life-threatening.
That said, some of the other conditions (comorbidities) associated with AS can be concerning. People with AS may be more likely to develop certain heart problems and osteoporosis. They may also be at risk for other inflammation-related conditions, such as inflammatory bowel disease (IBD), psoriasis and uveitis (eye inflammation) as well as mental health conditions like depression.
The outlook for AS is very good if addressed early in the disease course. With appropriate comprehensive treatment, including medications, physical therapy and exercise many people have preserved function and minimal pain.
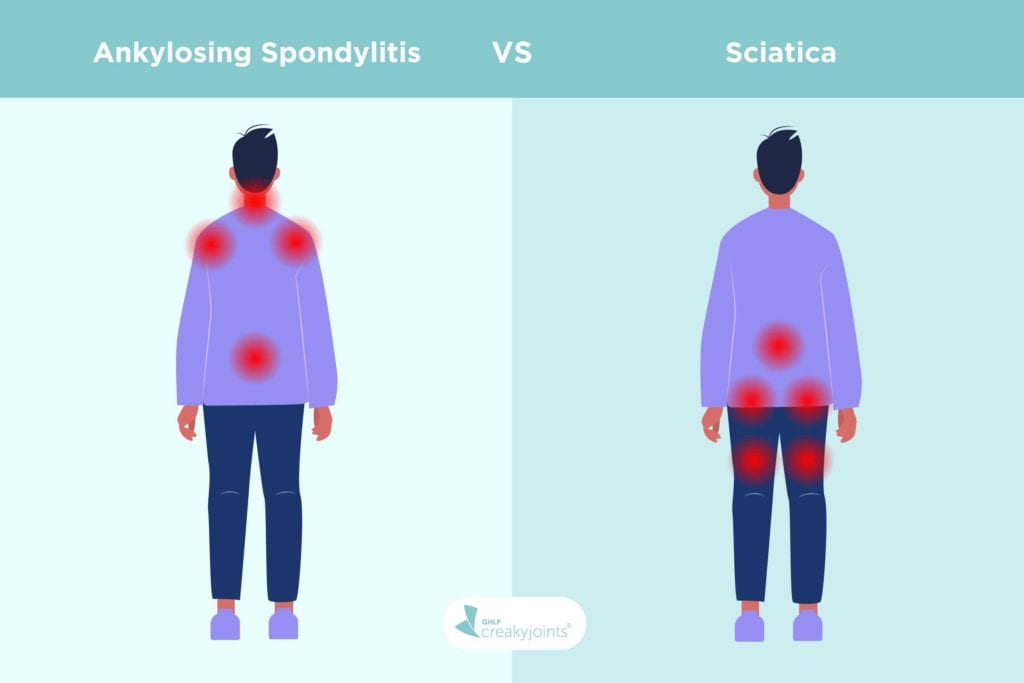
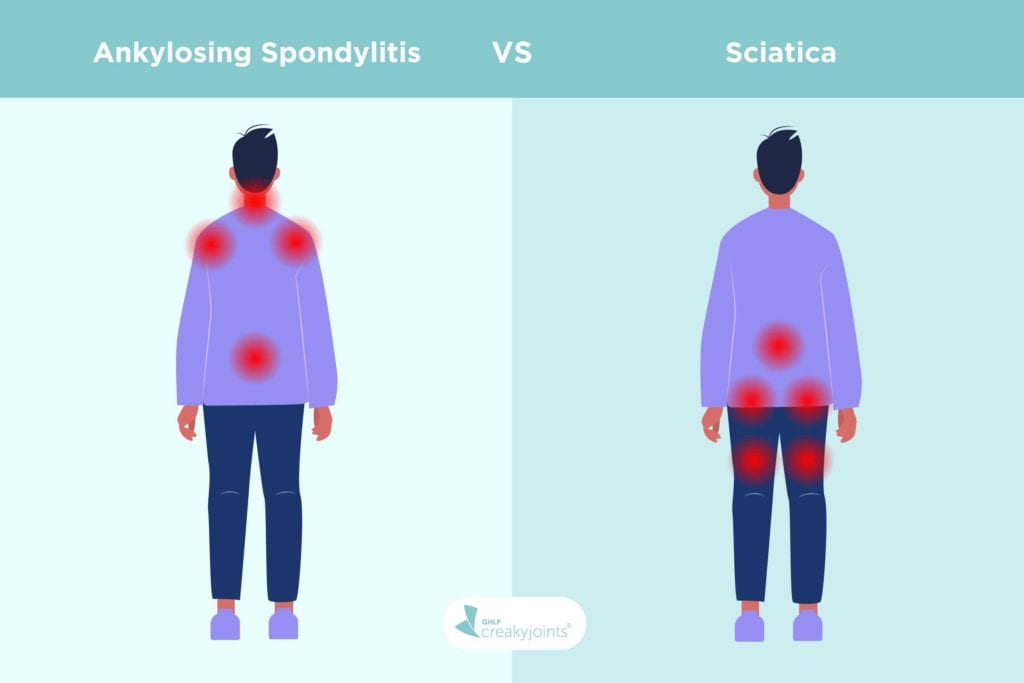
Ankylosing spondylitis symptoms
Ankylosing spondylitis can cause debilitating pain that can have a big impact on patients’ sleep, mood, ability to work and quality of life. Common AS symptoms include:
- Pain and stiffness in the lower back and hips.
- Pain and stiffness in other joints, such as the neck, shoulders or feet.
- Pain between the base of the spine and the pelvis.
- Pain that is worse in the morning gets better as you move around.
- Pain that improves after a hot shower.
- Alternating buttock pain.
- Difficulty breathing.
- Fatigue.
- Loss of appetite.
- Abdominal pain, diarrhoea and other gastrointestinal symptoms.
- Skin rash.
- Uveitis (eye inflammation).
Ankylosing spondylitis causes and risk factors
There isn’t one specific cause of AS, but there are known factors that can increase the risk for some groups. They are:
- Age and sex: AS usually develops between the ages of 15 and 45. It affects one in 200 people and is usually diagnosed many years (five to seven years on average) after the onset of symptoms. It was previously thought to be rare in women, but we now know women are often misdiagnosed and compromise around one-third of AS patients.
- Family history: People who have the HLA-B27 gene in their family are at greater risk of developing AS. That said, it is possible for people who don’t have this gene to develop the disease. And on the flip side, people who do carry the gene don’t always develop ankylosing spondylitis.
How ankylosing spondylitis is diagnosed
Doctors become more suspicious when you’ve had back pain that came on gradually and has lasted for at least three months. If your general practitioner thinks you might have AS, they can provide initial testing and then refer you to a rheumatologist for diagnosis. To help diagnose you, your doctor will:
- Talk to you about your risk factors and medical and family history: They will also ask about the nature of your back pain and other symptoms, such as when they started or what makes them feel worse or better.
- Conduct a physical exam to look for signs of spine fusion, inflammation and limited range of motion in your spine and other joints.
- Order imaging tests such as X-rays and MRIs, to get a better look at what’s happening with your spine and pelvic bones.
- Order blood tests to get more information about whether you are at risk of developing ankylosing spondylitis. These may include testing for the HLA-B27 genetic marker and looking for elevated levels of inflammation in the blood — erythrocyte sedimentation rate (ESR) or C-reactive protein (CRP).
How ankylosing spondylitis is treated
Once you have a confirmed diagnosis of AS, your rheumatologist will work out a treatment plan with you. Your plan will be designed to control inflammation and pain and to minimise joint damage. It will likely include an appropriate exercise regime, medication and lifestyle changes.
Your treatment plan will depend on other factors such as:
- Your current level of disease activity.
- How long you have had AS and your level of joint damage.
- Other related and non-related diseases you have.
- Whether some medications may cause you some harm. You and your treating doctor will need to weigh the risks of taking certain medications versus the risks of not taking them.
- Your personal preferences, such as medications that are taken as tablets, injections or infusions.
It is important to note that choosing not to treat your condition with evidence-based methods also has serious consequences — a very high risk of permanent joint damage, chronic pain and decreased function. This is because disease-modifying antirheumatic drugs (DMARDs) are the only proven way to slow or halt the progression and ease the symptoms of AS. Other treatments, such as anti-inflammatories and cortisone, may improve the symptoms, but they will not alter disease progression.
Understanding Sciatica
Sciatica can also cause back pain, but in a different way than ankylosing spondylitis. AS is a chronic inflammatory disease whereas sciatica is a mechanical issue that usually resolves with appropriate treatment.
The sciatic nerve branches from nerve roots in the lower spine through the hips and buttocks and down through the legs. It is the longest and thickest nerve in the body. Sciatica is nerve pain from damage or irritation to the sciatic nerve.
Sciatica causes and symptoms
Samar Gupta, MD, FACR, a rheumatologist at Michigan Medicine, explains that with sciatica, there tends to be a clear incident that triggered the pain. “(A person with sciatica may have) twisted their back, or bent in the wrong way,” he says. “Sciatica is very acute. For example, the person was fine yesterday and today they’re feeling horrible. But ankylosing spondylitis is different. They have this little backache that gradually gets worse.”
Although sciatica can cause intense pain, it isn’t necessarily something that requires serious medical intervention. Dr Gupta says most sciatica cases resolve within 90 days. That said, he also notes the importance of seeing a doctor if you suspect you could have sciatica, as it can cause permanent nerve damage if left untreated.
Your doctor can also help you rule out other causes of your back pain, such as AS or osteoarthritis.
Sciatica symptoms include:
- Sharp, burning pain that radiates from your lower spine down through your buttocks and the back of your leg, usually only on one side.
- Pain that is more felt in your lower leg compared to your lower back.
- Pain that worsens when you cough or sneeze.
- Pain that gets worse as the day goes on.
- Numbness, tingling or muscle weakness in the affected leg.
- Difficulty controlling your bowels or bladder (if this is the case, you should seek immediate medical care).
Sciatica causes and risk factors
Sciatica is a fairly common condition. About 40 per cent of US adults experience sciatica sometime in their life. Some people, however, are more at risk of experiencing sciatic pain because of their lifestyle and other health conditions. These risks include (but are not limited to):
- Previous injury: Having a slipped disk in your back can cause pressure on the sciatic nerve. Similarly, other back conditions can cause you to develop sciatica.
- Weight: People who are overweight can be at risk for sciatica because of the stress put on the spine.
- Job: Having a labour-intensive job that requires you to twist your back or carry heavy loads may increase your risk of developing sciatica.
- Diabetes: Having diabetes increases your risk of nerve damage, which can make it more likely for you to have sciatica.
- Osteoarthritis: As osteoarthritis breaks down the cartilage that cushions your bones, your body can grow bone spurs to try and repair the loss. These bone spurs can form in your spine and press on your sciatic nerve.
- Weak core: Having well-developed back and core muscles helps support the spine, which in turn decreases your risk for sciatica.
- Age: Age-related changes in the spine can be a common cause of sciatica.
- Smoking: Nicotine can damage spinal tissue and weaken bones, meaning people who smoke may be more likely to develop sciatica.
How sciatica is diagnosed
Your doctor will check your medical history and ask you to walk on your heels or toes or to perform other movements to check for pain, flexibility and muscle strength or to test your reflexes.
In some cases, such as instances where sciatica doesn’t resolve within a normal timeframe, your doctor may order more tests. These could include x-rays, CT scans or MRI scans to look for bone obstructions or other conditions that may be causing your sciatica.
How sciatica is treated
If your doctor diagnoses you with sciatica, there are several treatment options they may recommend.
- Ice/heat therapy: Apply an ice pack or heat pack to the painful areas throughout the day may give you some relief. Ice packs reduce swelling and should only be used for 15 to 20 minutes at a time. Heat packs relax muscles and can be used longer if they are not too hot.
- Physical therapy: Your doctor may recommend physical therapy to treat your sciatic pain. A physical therapist can perform and teach gentle stretches or exercises that will help your core muscles support your back. They may also recommend light exercise, like walking or swimming.
- Medications: Some of the medications used to treat sciatica can include muscle relaxants, anti-inflammatory drugs or painkillers.
- Spinal injections: If needed, your doctor might recommend getting epidural injections of a corticosteroid medication in the area around the nerve root that is causing you trouble. This can help suppress inflammation around the irritated nerve and reduce pain.
- Surgery: In severe cases, your doctor may consider surgery to treat sciatica. A severe case would be if you experience loss of bladder or bowel control or significant weakness, or if no other therapy/treatment has improved your condition. A surgeon may be able to remove the bone spur or part of the disk that’s causing pain, but this is usually a last resort.
Does Ankylosing Spondylitis Cause Sciatica?
Although both conditions can cause back pain, one ailment doesn’t cause the other one to occur, except in very unusual cases.
“Ankylosing spondylitis causing sciatica is not impossible, but it’s a very rare occurrence,” explains Dr Gupta. “The opposite is not true — sciatica doesn’t cause ankylosing spondylitis.”
He notes that sacroiliitis — inflammation of the sacroiliac joint, which is where the spine connects with the pelvis and is a common feature of ankylosing spondylitis — causing symptoms of sciatica has been reported in a handful of cases.
This information should never replace the information and advice from your treating doctors. It is meant to inform the discussion that you have with healthcare professionals, as well as others who play a role in your care and well-being.
This page content has been modified, with permission, from a corresponding article by Jamie Ballard on the CreakyJoints US website. Some content may have been changed to suit our Australian audience.
Keep Reading
A Patient’s Guide to Living with Axial Spondyloarthritis in Australia
Sources
Interview with Samar Gupta, MD, FACR, a rheumatologist at Michigan Medicine
Cleveland Clinic — Sciatica https://my.clevelandclinic.org/health/diseases/12792-sciatica
Harvard Health — Back pain: What you can expect from steroid injections https://www.health.harvard.edu/pain/back-pain-what-you-can-expect-from-steroid-injections
healthdirect — Epidural injection for chronic pain relief https://www.healthdirect.gov.au/surgery/epidural-injection-for-chronic-pain-relief
Mayo Clinic — Sciatica https://www.mayoclinic.org/diseases-conditions/sciatica/symptoms-causes/syc-20377435
myDr — Exercise & Fitness, Symptoms. Sciatica: symptoms, causes and diagnosis https://www.mydr.com.au/symptoms/sciatica-symptoms-causes-and-diagnosis/
Spondylitis Association of America — Spondy What? https://spondylitis.org/
V Golder and L Schachna. Ankylosing spondylitis: An update. Australian Family Physician. Volume 42, Issue 11, November 2013 https://www.racgp.org.au/afp/2013/november/ankylosing-spondylitis/





