People with rheumatoid arthritis (RA) who are prescribed corticosteroids such as prednisone often have questions and concerns about them. And it’s not hard to see why: These medications come with a long list of side effects, ranging from insomnia and weight gain to high blood sugar and thinning bones. But when corticosteroids like prednisone are judiciously in the right patients, these drugs can be safe and effective, according to Anthan Tiliakos, DO, an assistant professor in the division of rheumatology at Emory Healthcare in Atlanta.
“There is some controversy in rheumatology about the use of drugs like prednisone, and some doctors believe they have no place in the treatment of RA,” he says. “I’m of the opinion that it can be an excellent medication in certain circumstances.”
To help improve the understanding of how prednisone — and other corticosteroids such as dexamethasone and methylprednisolone — can help control rheumatoid arthritis, we asked Dr. Tiliakos to answer some of the most common questions and concerns patients have about the drug.
1. What Are Corticosteroids?
Corticosteroids, or steroids, are a type of steroid hormone used to treat many types of conditions besides RA, such as asthma, Crohn’s disease, and multiple sclerosis. Prednisone is one of the drugs in a class of corticosteroids called glucocorticoids, which reduce inflammation and suppress the immune system. When used in RA patients, prednisone is typically given orally, but injections of prednisone are sometimes used in those who have nausea or have difficulty swallowing, Dr. Tiliakos says. If a patient needs to take a high dose of the drug, it may be given intravenously.
While corticosteroids are a steroid hormone, rest assured that they’re not the same as anabolic steroids, which are sometimes abused by athletes and bodybuilders to build muscle mass and improve performance. Anabolic steroids are synthetic versions of male sex hormones and are generally only prescribed to boys with delayed puberty or to men with conditions linked to low testosterone.
2. How Do Corticosteroids Like Prednisone Work to Improve RA Symptoms?
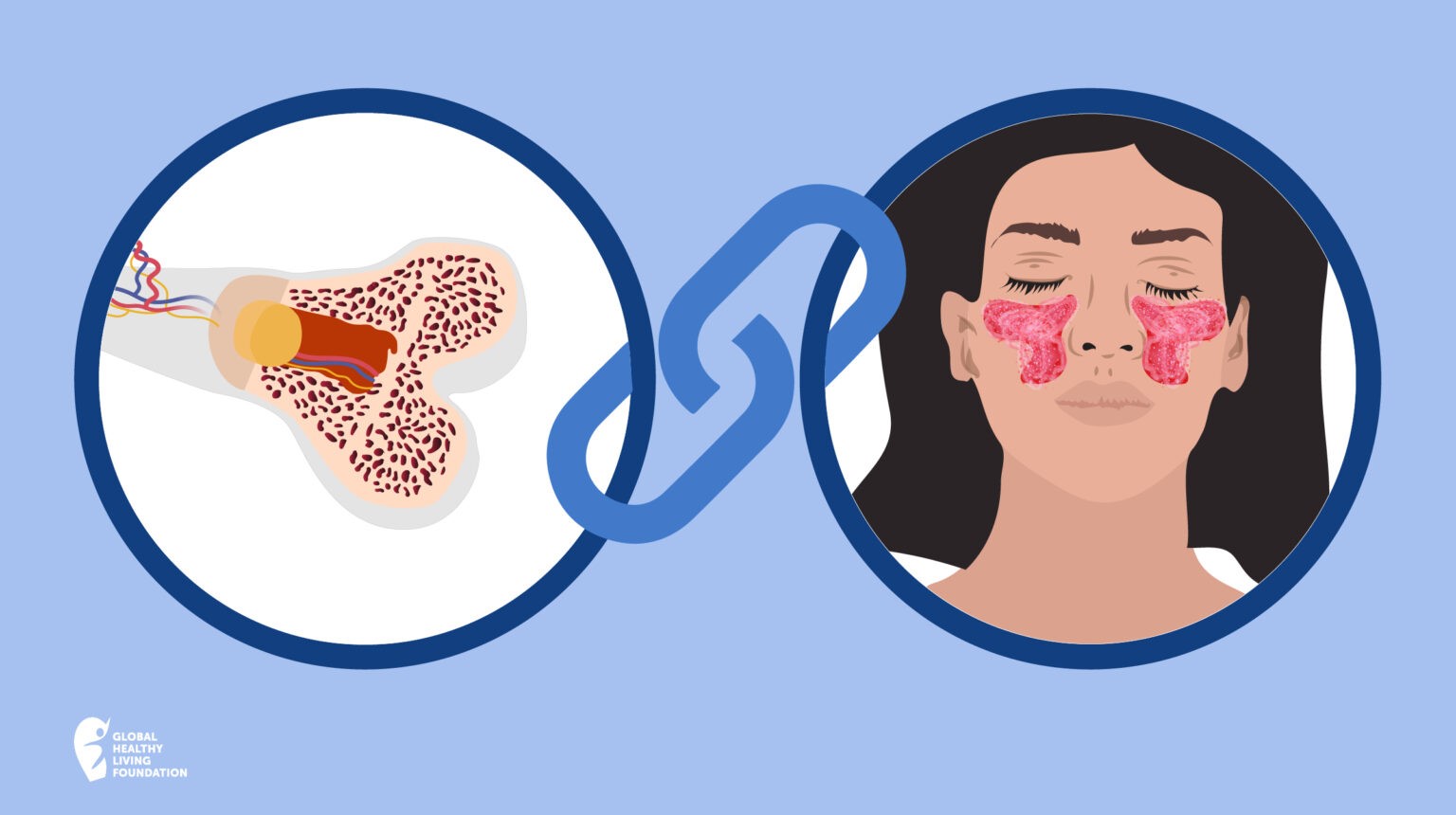
Dr. Tiliakos says there are two ways these medications are thought to work. One is by stopping the production of certain pro-inflammatory cytokines. These immune system molecules are involved in both joint inflammation and erosion of the bone that occurs in RA.
“Prednisone stimulates the glucocorticoid receptors in the cells, which causes suppression of these harmful cytokines,” Dr. Tiliakos explains. “This reduces inflammation and the pain and stiffness associated with it.”
The second way is that glucocorticoids like prednisone also act like COX-2 inhibitors, which are nonsteroidal anti-inflammatory drugs (NSAIDs) that target cyclooxygenase-2, an enzyme responsible for pain and inflammation.
Prednisone may even help limit the joint damage that occurs in RA, Dr. Tiliakos says: “There’s evidence that it acts like a DMARD, or a disease-modifying antirheumatic drug, to slow progression of the disease.”
3. When Is Prednisone Typically Prescribed for People with RA?
Because prednisone starts working so quickly, one of its most common uses is providing a “bridge therapy” for people in the early stages of RA, Dr. Tiliakos says. “DMARDs take quite a while to kick in, and it’s not fair to have a patient struggle with their symptoms for weeks while we wait for the medication to start working,” he explains. (Prednisone can safely be used with both conventional DMARDs, such as methotrexate, and biologics.)
Prednisone is also helpful for RA patients who are experiencing a severe flare, he adds: “It allows you to regain control of the disease relatively quickly.” Prednisone may also be prescribed to patients who haven’t responded well to DMARDs or biologics.
4. Doesn’t Prednisone Have a Lot of Side Effects?
It does, though the side effects of prednisone depend on the strength of the dose and for how long you take it. Side effects of prednisone range from gastrointestinal upset (diarrhea, stomach pain) and neurologic/psychiatric (mood swings, insomnia) to ophthalmic (blurred vision, cataracts) and endocrine (diabetes, hyperglycemia.) Taking prednisone can dramatically weaken your bones, leading to osteoporosis, may cause cravings that cause weight gain, and can increase your risk of infections.
This is why rheumatologists always try to keep patients on the lowest dose possible.
“One big misconception people have is that the side effects of taking 5 or 10 mg of prednisone are as severe as those of 60 mg,” Dr. Tiliakos says. “While we do see certain side effects of concern in people on low doses — such as osteopenia, bruising, weight gain, and gastrointestinal symptoms — we have ways to mitigate those.”
If you’re prescribed prednisone or another glucocorticoid, your doctor will likely recommend you take certain steps to limit these side effects, such as avoiding NSAIDs (which can exacerbate GI symptoms) and taking calcium and vitamin D to help strengthen your bones.
5. How Long Can Prednisone Safely be Used?
Unfortunately, there’s no simple answer. Experts know that the risk of serious side effects of taking prednisone, such as osteoporosis and diabetes, increases with long-term use and higher dosages. What’s controversial among rheumatologists, Dr. Tiliakos says, is whether patients can safely take low doses of prednisone (10 mg or less daily) for long periods of time.
“Some say it’s okay for an RA patient to take 5 mg of daily for years if need be, while others think prednisone is dangerous and want their patients off it completely,” Dr. Tiliakos says. “I’m of the school of thought that it’s acceptable to take 5 mg for long periods of time, though it depends on the patient.”
The good news is that most people with RA can be sufficiently treated with just 5 to 10 mg of prednisone, he adds. Larger doses of prednisone — which can be as high as 60 mg a day — are more likely to be used in RA patients who are experiencing extra-articular symptoms such as eye or lung inflammation. (Learn more about uveitis and arthritis and how lungs are affected by arthritis here.)
6. Why Is It So Important to Taper Prednisone When You Stop Taking It?
If your rheumatologist says you may be able to stop taking prednisone or cut your dosage, don’t be tempted to speed up the recommended weaning process. Not tapering prednisone properly can lead to adrenal insufficiency, a condition in which the body doesn’t produce enough of the hormone cortisol.
“The adrenal glands make a natural amount of steroids every day, and if you’re on a glucocorticoid like prednisone for a long period of time, the adrenal glands may shut down or go to sleep for a little while,” Dr. Tiliakos says. “Tapering prednisone is an attempt to ‘wake up’ your adrenal glands so they can start doing their job again.”
In fact, one of the reasons prednisone is prescribed more often than other glucocorticoids is because it’s available in so many dosages, which makes it easier to taper by smaller increments if necessary, he adds.
Keep Reading
- Glucocorticoids and Infection Risk: What You Need to Know
- Steroid Injections for Arthritis: How to Prepare
- The 4 Stages of Rheumatoid Arthritis Progression