On 16 February 2023, the Australian Rheumatology Association updated the following Patient Information on the COVID-19 vaccination in autoimmune inflammatory rheumatic diseases (AIRD).
This information should never replace the information and advice from your treating doctors. It is meant to inform the discussion that you have with healthcare professionals, as well as others who play a role in your care and well-being.
Why is it Important For Me to Have the COVID-19 Vaccine?
Some diseases (including rheumatoid arthritis) are caused by the body’s immune system, which usually protects us from infection. When the immune system is affected by arthritis or drugs to treat the condition, the risk from COVID-19 may be increased.
If you get vaccinated, you will be less likely to get COVID-19. Even if you do get COVID-19 when vaccinated, it is more likely to be a milder illness.
People who catch COVID-19 can become very unwell. There is a large amount of information that confirms being unvaccinated not only makes you more likely to get infected but also that you are more likely to become sick or die if you are infected.
For more practical tips for patients in the COVID-19 pandemic, see: Practical Tips for people with Rheumatoid Arthritis, SLE and other AIRD in the COVID pandemic.
What Vaccines Are Available?
Six COVID-19 vaccines are currently available in Australia – AstraZeneca (Vaxzevria/Oxford), Moderna (Spikevax), Moderna (Spikevax) Bivalent, Novavax (Nuvaxovid),Pfizer (Comirnaty) and Pfizer (Comirnaty) Bivalent vaccines. All of these are suitable for rheumatology patients whose immune system may not be strong. The AstraZeneca vaccine is a viral vector vaccine. The Pfizer and Moderna vaccines use messenger RNA (mRNA). Novavax vaccine is a spike protein-based vaccine.
Which Vaccine Should I Have?
The COVID-19 vaccines available in Australia are safe for people with arthritis and people taking drugs that suppress the immune system, even if the condition is active. This is because none of these is a “live” vaccine.
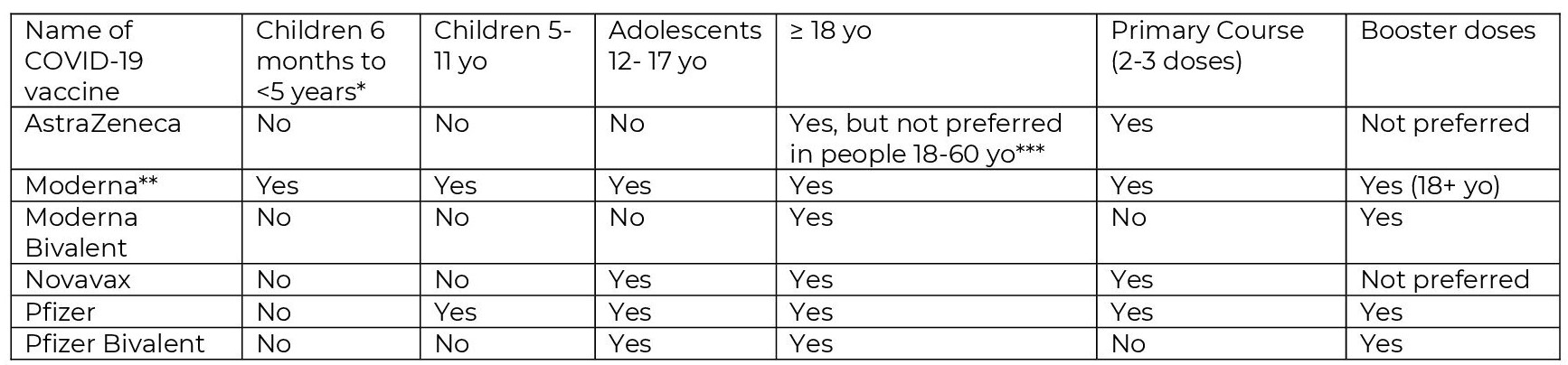
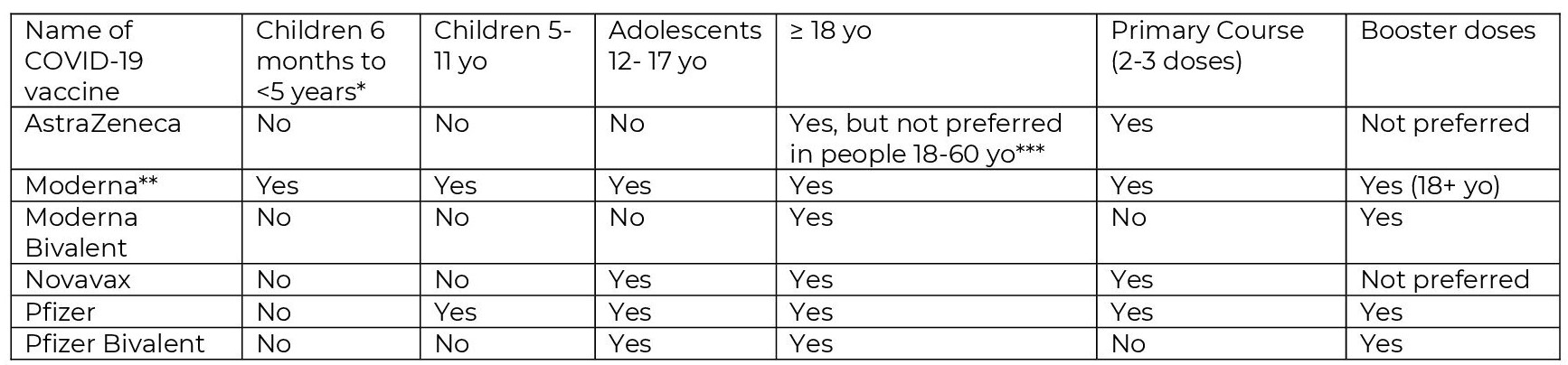
* Children aged 6 months to <5 years with severe immunocompromise, disability, and those who have complex and/or multiple health conditions which increase the risk of severe COVID-19.
** Severely immunocompromised people who are receiving a third primary dose of the Moderna vaccine should receive a 100mcg dose. When Moderna is used as a booster the recommended dose is 50mcg (i.e. half the dose used for the primary course).
*** The AstraZeneca vaccine can be used in adults aged 18-60 years where the benefits are likely to outweigh the risks for that individual and the person has made an informed decision based on an understanding of the risks and benefits.
People over the age of 60 can receive any of the COVID-19 vaccines (provided that they don’t have the conditions listed below) as the benefits of the AstraZeneca vaccine continue to outweigh the risk of adverse effects in this age group.
AstraZeneca (Vaxzevria) is not recommended in patients with: a history of cerebral venous sinus thrombosis (CVST), a past history of heparin-induced thrombocytopenia (HIT), a past history of idiopathic splanchnic (mesenteric, portal, splenic) vein thrombosis and antiphospholipid syndrome with thrombosis.
People who have had their first dose of the COVID-19 AstraZeneca vaccine without any serious adverse events or allergic reactions can safely be given their second dose. This includes adults under the age of 60.
The Pfizer and Moderna vaccines should not be given if you have had a serious adverse event (including myocarditis and/or pericarditis) or an allergic reaction to a previous dose. In some people with rare inflammatory heart disorders (e.g., recent or current myocarditis, endocarditis, pericarditis or rheumatic fever) or severe heart failure, the mRNA vaccines (Moderna and Pfizer) may not be suitable. Discuss with your specialist if you have concerns.
Note that the mRNA vaccines are safe to use in people with most common forms of heart disease (including angina or a history of heart attacks). The risk of myocarditis or pericarditis following the Pfizer bivalent and Moderna bivalent vaccine has not yet been characterised, as these vaccines have not been used extensively in large populations. However, there is no reason to believe the safety of the Pfizer bivalent and Moderna bivalent vaccines are any different to other Pfizer/Moderna mRNA vaccines.
If you have had an allergic reaction to a previous vaccine, let your healthcare team know as you should not receive a dose of that same brand of vaccine again.
Protection From COVID-19
All the vaccines are very good at stopping severe symptoms and hospitalisation caused by COVID-19 after the initial primary course (2-3 doses) and the necessary booster doses.
Primary Course
How many doses do I need?
All the vaccines require a second primary dose:
- AstraZeneca usually 4-12 weeks after the first dose.
- Moderna vaccine usually
- 8 weeks after the first dose for people 5+ years (particularly males aged 12-39 years) or for children aged 6 months to < 5 years at risk of severe COVID-19.
- 4 weeks after the first dose for people who are moderately or severely immunocompromised, at risk of severe disease or aged 65+ years).
- Pfizer vaccine usually
- 8 weeks after the first dose for people 5+ years (particularly males aged 12-39 years).
- 3 weeks after the first dose for people who are moderately or severely immunocompromised, at risk of severe disease or aged 65+ years)
- Novavax vaccine usually 3 weeks after the first dose.
The first dose does provide some protection. The second dose gives more long-term protection from COVID-19. Some people require a third dose to complete their primary course.
What is a Third Primary Dose and How is it Different to a Booster Dose?
A third primary dose is recommended to be given 2 months (28 days can be considered in exceptional circumstances) after the second dose in people who may not have had a strong immune response to the 2 initial doses due to their medical conditions and/or medications. This third primary dose “completes the primary course” for these people. Some, but not all with AIRD on immunosuppressant therapy will fall into this category.
A third primary dose is different to a booster dose. See “booster doses” below.
Do I Need a Third Primary Dose?
Not all people with rheumatological diseases will need a third primary dose, however ATAGI are recommending a third primary dose for people who might not have had a complete response to the first two doses due to the use of the following immunosuppressive therapies:
- High dose corticosteroid treatment equivalent to >20mg/day of prednisone for ≥14 days in a month, or pulse corticosteroid therapy
- Multiple immunosuppressants where the combination is considered to be severely immunosuppressive
- At least one of the following conventional synthetic DMARDs:
- methotrexate (>10mg/week)
- leflunomide
- mycophenolate
- azathioprine (>1mg/kg/day)
- cyclosporine
- cyclophosphamide
- tacrolimus
- At least one of the following biological or targeted synthetic DMARDs:
- janus kinase (JAK) inhibitor (for e.g., baricitinib, tofacitinib, upadacitinib)
- abatacept
- rituximab
Some other treatments or combinations of treatments and/or conditions might also qualify for a third primary dose of vaccine – ask your specialist or GP if you are uncertain.
- Moderna or Pfizer are preferred for the third primary dose however you can receive Novavax for your third primary dose if you have received Novavax for your first 2 doses, and AstraZeneca if you can’t have the mRNA vaccines.
- The third primary dose is usually given 2 months after the second dose of vaccine (28 days can be considered in exceptional circumstances).
- Talk to your rheumatologist about the timing of your medicines around your third primary dose as you did with the previous doses.
The ATAGI recommendations can be found here; https://www.health.gov.au/news/atagi-statement-on-the-use-of-a-3rd-primary-dose-of-covid-19-vaccine-in-individuals-who-are-severely-immunocompromised
Booster Doses
A booster dose refers to an additional vaccine dose after the primary vaccine course is complete which for most people is 2 doses. A booster dose is recommended for individuals who have completed their primary course, 3 or more months ago:
- For all individuals aged 16 years and above
- For adolescents aged 12-15 years who are severely immunocompromised, have a disability with significant or complex health needs or multiple health conditions that increase the risk of severe COVID-19 (Pfizer vaccine only).
In line with recommendations for the entire community, all patients with AIRD should have had a booster dose after they completed their primary course (regardless of whether this was a 2-dose or 3-dose primary course). Many people with AIRD will have had a 2022 winter booster dose. A third booster dose (the “2023 booster dose) is now recommended for certain people. This will mean that some people with rheumatic diseases will be up to their 6th dose COVID-19 vaccine dose i.e. a primary course of 3 doses, original booster, 2022 winter booster and the 2023 booster dose.
The third booster dose is recommended for the following people if their last COVID-19 vaccine dose or confirmed COVID infection (whichever is the most recent) was > 6 months ago and regardless of the number of prior doses received;
- All adults > 65 years
- Adults 18-64 years who have medical co-morbidities that increase their risk of severe COVID-19 (for e.g. severe immunocompromise), or disability with significant or complex health needs
A third booster dose should be considered in the following people if their last COVID-19 vaccine dose or confirmed COVID infection (whichever is the most recent) was > 6 months ago and regardless of the number of prior doses received;
- All Adults aged 18-64 years without risk factors for severe COVID-19
- Children and adolescents aged 5-17 years who have medical comorbidities that increase their risk of severe COVID-19 (for e.g. severe immunocompromise), or disability with significant or complex health needs.
If you are unsure whether you should have a 2023 booster dose, speak to your rheumatologist or doctor.
Which Brand of Vaccine Should I Have For My Booster Dose?
Any of the vaccines listed above can be used for booster doses. While both bivalent and original vaccines result in an immune response against some of the Omicron strains (BA.1 and BA.4/BA.5), the Pfizer and Moderna bivalent vaccines have been shown to be slightly more effective compared to the original vaccines. If you have not yet had your booster doses talk to your health professional about the best vaccine for you.
Will the Medicines That I Take For My Condition Affect the Way the Vaccine Works?
Some people who are taking medicines that suppress the immune system may be given advice to continue avoiding exposure to COVID-19 after they have had the vaccine. This is because their medications could mean their immune system does not respond as strongly to the vaccine as people who don’t take these drugs. This does not mean you should stop your treatment, because this can result in a flare of your condition which puts you at greater risk from COVID-19. Everyone in Australia will need to follow Government advice on reducing the spread of COVID-19, even after they have had the vaccine.
Can I Have Other Vaccines (e.g. Influenza Vaccine) at the Same Time as the COVID-19 Vaccine?
Yes, the COVID-19 vaccine and the influenza (flu) vaccine can be safely given on the same day.
You do not need to delay your influenza vaccine until you complete the course of COVID-19 vaccines, in fact the COVID-19 vaccine does not protect against the flu, so it is important to still have your annual flu vaccine.
Should I Delay My Rituximab Treatment So That I Can Have the COVID-19 Vaccine?
To ensure the best response to the COVID-19 vaccine, it is recommended that vaccination is performed towards the end of a rituximab dosing cycle or before initiation of rituximab therapy. Please discuss the timing with your rheumatologist as it is extremely important to maximise the benefit of the vaccine.
Should I Continue to Take Methotrexate When I Have the COVID-19 Vaccine?
There is some evidence that responses to the COVID-19 vaccine are reduced in people treated with methotrexate. Therefore, interruption of methotrexate therapy during COVID-19 vaccination may be considered, but only in patients with stable rheumatic disease at low risk of flare, or those for whom protection from COVID-19 is of particular importance. This decision to hold methotrexate for one or two doses following each vaccination should be individualised and discussed with your treating rheumatologist.
More information on the use of other immunomodulatory medicines with the COVID-19 vaccine is available here: https://anzmusc.org/wp-content/uploads/2021/11/Clinician-guide-for-the-use-of-immunomodulatory-drugs-in-autoimmune-rheumatic-diseases-at-the-time-of-COVID-19-vaccination-v1.1-20211108.pdf
Can I Have the COVID-19 Vaccine If I am Pregnant or Breastfeeding?
The Australian Government recommends the use of either the Moderna, or Pfizer vaccines for both the primary and booster doses in pregnant women at any stage of their pregnancy. This is because the risk of severe outcomes from COVID-19 is significantly higher for pregnant women and their unborn baby. There is still limited data on the safety of the AstraZeneca and Novavax vaccines in pregnancy. Women who are trying to become pregnant do not need to delay vaccination or avoid becoming pregnant after vaccination. A shared decision making guide for women who are pregnant, breastfeeding or planning a pregnancy can be found here: https://www.health.gov.au/resources/publications/covid-19-vaccination-shared-decision-making-guide-for-women-who-are-pregnant-breastfeeding-or-planning-pregnancy
All 6 vaccines can be given to women who are breastfeeding. Breastfeeding women do not need to stop breastfeeding to receive the vaccine. More information can be found here; https://ranzcog.edu.au/RANZCOG_SITE/media/RANZCOG-MEDIA/News/RANZCOG-ABA-NZBACOVID-19-vaccination-and-breastfeeding-infographic-final.pdf. You can talk to your midwife and/or rheumatology healthcare team if you are not sure what to do.
Are There Any Side Effects?
Some people will get mild side effects. These can include pain at the injection site, tiredness, headache and aching of muscles. Serious reactions like allergic reactions are extremely rare. People with a history of severe allergic reactions can be vaccinated but should be monitored for 30 minutes after receiving the vaccine. If you have any concerns about the vaccine, ask your doctor, nurse or pharmacist.
You should seek medical advice as soon as possible if:
- You have any of the following symptoms, particularly around 4 to 42 days after vaccination with AstraZeneca: headache that persists beyond 48 hours after vaccination or appears later than 48 hours after vaccination, blurred vision, weakness of face or limbs, confusion or seizure, shortness of breath, chest pain, persistent abdominal pain, leg swelling or a pinprick rash or bruising not at the injection site that cannot be explained.
- You experience chest pain, pressure or discomfort, irregular heartbeat, skipped beats or ‘fluttering’, fainting, shortness of breath or pain when breathing.
If I Didn’t Have a Side Effect Does This Mean That the Vaccine Didn’t Work?
Not everybody will have side effects from the COVID-19 vaccine. If you don’t get any side effects this does not mean that the vaccine did not work.
Thrombosis with thrombocytopenia syndrome (TTS) can now be treated very effectively. Due to better awareness, early diagnosis and appropriate treatment, the outcome and prognosis of the majority of those who have experienced this syndrome is good. More information can be found here; https://www.health.gov.au/news/joint-statement-from-atagiand-thanz-on-thrombosis-with-thrombocytopenia-syndrome-tts-and-the-use-of-covid-19- vaccine-astrazeneca
Do You Still Need to Have the Vaccine if You Have Had COVID-19?
People who have had COVID-19 should be vaccinated with a COVID-19 vaccine. This provides extra protection against future infections. Wait for 6 months after COVID infection or previous dose of COVID vaccine before receiving the 2023 COVID-19 vaccine booster dose.
Please encourage your household members and other close contacts to have all the recommended COVID-19 vaccinations, including the booster doses once they are eligible as this may offer you further protection from getting COVID-19. This is known as the “ring” vaccination concept.
An Australian Government COVID vaccine fact checker is available at; https://www.health.gov.au/initiatives-and-programs/covid-19-vaccines/is-it-true
More information for your treating doctors can be found here. https://anzmusc.org/wp-content/uploads/2021/11/Clinician-guide-for-the-use-of-immunomodulatory-drugs-in-autoimmune-rheumatic-diseases-at-the-time-of-COVID-19-vaccination-v1.1-20211108.pdf
https://app.magicapp.org/#/guideline/LqRV3n/rec/EZ6z8E/practical
https://www.health.gov.au/news/atagi-2023-booster-advice
The ARA will update this advice as new information becomes available.
The information in this document has been obtained from various sources and has been reviewed by the Australian Rheumatology Association. It is intended as an educational aid and does not cover all aspects of the topic. This information is not intended as medical advice for individual problems nor for making an individual assessment of the risks and benefits. It can be reproduced in its entirety but cannot be altered without permission from the ARA.
The information above is correct as of 16 February 2023.
Keep Reading
- GHLF Australia: COVID-19 self-care guide: Essential pre-planning information for people with chronic conditions
- Living With Arthritis During COVID-19: Education and Support Resources
- Patient Guidelines for Living With Arthritis in Australia
- Patient PrepRheum podcast
- GHLF Australia: MatterofVax: Vaccination Facts and Resources




