Biologic DMARDs
What Are Biologics?
Biologic DMARDs (also called bDMARDs or “biologics”) are a class of disease-modifying antirheumatic drugs (DMARDs). They are grown from biologically-sourced cells.
Biologics have very large molecular structures compared to those of tablet-form medications. (Picture a basketball next to a pea and you’ll get the idea.) As a result, they cannot be processed through the digestive system. Instead, they are injected or infused into the bloodstream.
Due to their complex nature, biologics are difficult to copy with 100 per cent accuracy. They can even vary slightly between batches.
How Do Biologics Work?
Biologics are designed to act like the proteins that are already in your body. They target specific areas of your immune system. Because they are so specific, they may cause fewer side effects than conventional synthetic DMARDs. However, like other DMARDs, they can increase your risk of infection.
Why Have I Been Prescribed a Biologic?
Your rheumatologist may prescribe a biologic if your previous csDMARD therapy was ineffective or if you cannot take conventional DMARDs. Personal considerations such as comorbidities and side effects may make a biologic (often with the addition of methotrexate) a possible option for you.
Biologics can be prescribed for many types of autoimmune arthritis, such as rheumatoid arthritis, ankylosing spondylitis and psoriatic arthritis.
They are heavily subsidised through the Pharmaceutical Benefits Scheme (PBS). A biologic will only be prescribed if your condition is active and csDMARD treatment is unsuccessful or inadequate. Access will only be continued if the biologic helps your condition.
Only rheumatologists and clinical immunologists are authorised to prescribe bDMARDs in Australia.
You can only be prescribed one biologic or targeted synthetic DMARD/JAK inhibitor at a time as such intense suppression of the immune system is considered too great to be risked and the extra benefits too insignificant.
How Soon Will I See the Benefits of Biologics?
The benefits of biologics are usually seen within a few weeks (but can take up to 12 weeks), unlike csDMARDs, which can take up to a few months to take effect.
How Will I Take My Biologic?
You may be able to give yourself this medication — via subcutaneous injections — at home (known as “self-injection”). You can also receive it via an infusion in a hospital or authorised infusion centre. You and your doctor can decide if an infusion is the right option for you. The infusions can last as little as 30 minutes or could take up to several hours — depending on the medication, dose and individual.
Self-injecting device options may include an auto-injector pen or a pre-filled syringe. A healthcare professional will indicate where on your body it is safe to administer these injections (usually the upper leg or stomach). Make sure to rotate the injection sites.
If you have psoriasis, do not inject in affected areas. Tell your prescribing doctor if you have an allergy to latex, as the needle cover on the pre-filled syringe and the injector pen contains dry natural rubber.
If you’re afraid to inject yourself, talk to your rheumatologist or their clinic staff about having someone available to give you these shots. Alternatively, you may ask a trusted friend or family member to administer them to you. If someone else injects you, ensure they have been trained to do so.
Many biologic drug suppliers have a patient support program in place. Through these, you can arrange for a nurse to come to your home and show you how to self-inject safely and to answer your questions. Be sure you are confident on how to do this procedure before you administer the medication on your own. Don’t be afraid to ask for help!
Classification of Biologics
There are two main classes of biologic DMARDs; each targets slightly different parts of the immune system:
- TNFi biologics (Adalimumab, Humira®, Certolizumab, Cimzia®, Etanercept, Enbrel®, Golimumab, Simponi®, Infliximab, Remicade®)
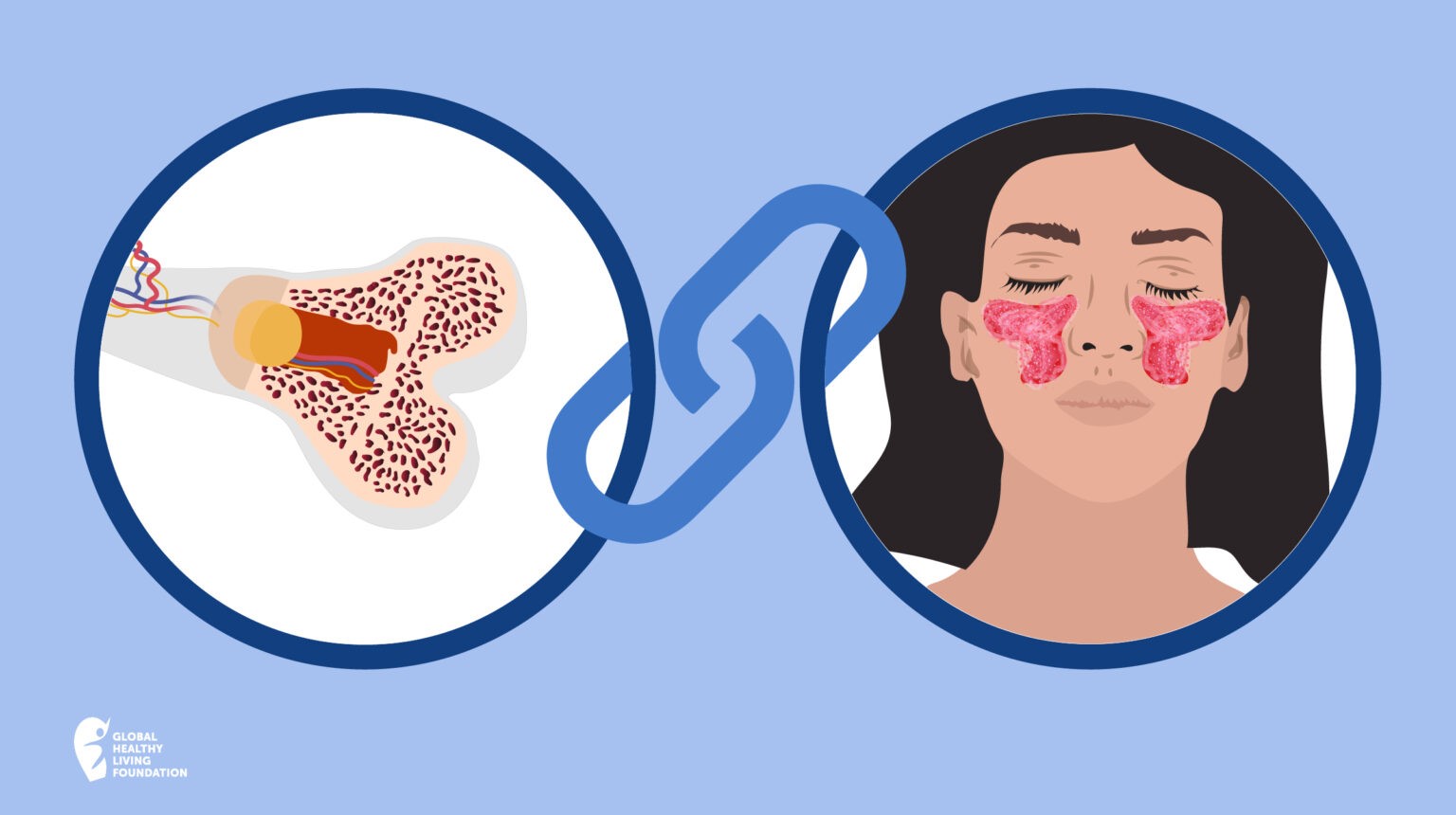
TNFi biologics work by targeting something called tumour necrosis factor proteins, or TNF. TNF is a protein that sends signals to your body, eventually leading to inflammation that causes swelling, pain and stiffness. By inhibiting, or stopping, TNF, these medications can reduce inflammation. They are also often simply called TNF inhibitors. - Non-TNFi biologics (Abatacept, Orencia®, Rituximab, MabThera®, Tocilizumab, Actemra®)
Non-TNFi biologics include a range of other biologics that target the immune system in different ways from TNFi medications. They interact with different kinds of white blood cells, such as T-cells or B-cells, in your immune system. They can also block chemicals called cytokines that cause inflammation.
There’s another medication option that is now available in Australia to treat some forms of inflammatory arthritis — biosimilar medications. You may have seen this term in the news, or even heard your doctor or nurses mention it. Biosimilars work the same way as biologics and have the same indications, however, the approval processes currently differ.
As original biologic brand patents expire, very close copies of these (known as biosimilars) are now coming onto the market. However, they are not technically considered generic medications (which are 100 per cent identical in structure to their original synthetic medication counterparts).
Biosimilars use the research already completed by the original biologic manufacturer and build on this, so they require comparatively less time and clinical trial data to receive approval. They are available for a range of conditions, including types of inflammatory arthritis.
Biosimilars are taken in the same way as their reference medication (including how they are used before, during and after pregnancy), and have the same possible side effects, contraindications and monitoring tests. All biosimilars have to meet the same standards of safety and efficacy as any other prescription medication approved by the Therapeutic Goods Association (TGA).
The biosimilars for inflammatory arthritis that are currently subsidised in Australia through the Pharmaceutical Benefits Scheme (PBS) are:
- Infliximab (Inflectra®, Remsima®, Emisima®, Flixceli®, Renflexis®)
- Etanercept (Brenzys®, Erelzi®)
- Adalimumab (Hyrimoz®, Hadlima®, Amgevita®, Idacio®)
Arthritis treatment information is also included in all editions of the CreakyJoints Australia Raising the Voice of Patients series. Learn more or download your free copy of A Patient’s Guide to Living with Rheumatoid Arthritis in Australia or A Patient’s Guide to Living with Axial Spondyloarthritis in Australia today.
For more information about biosimilars, the Therapeutic Goods Administration (TGA), Pharmaceutical Benefits Scheme (PBS) and much more, listen to the relevant episodes of our Patient PrepRheum podcast series or read the transcriptions attached to each episode.