For people with autoimmune conditions like rheumatoid arthritis (RA), psoriatic arthritis (PsA) or ankylosing spondylitis (AS), finding the right medication regimen often takes months or even years. It is common for patients to become frustrated and discouraged with this experience (and this is on top of the delays that most patients have to endure to get diagnosed in the first place).
Getting early and appropriate treatment can make a major difference for people living with these conditions. The trial and error process of finding the right medication can exacerbate symptoms, cause disease progression, and reduce quality of life.
Thankfully, current research in the field of rheumatology is examining how to better tailor treatment plans and determine which kinds of medication are more likely to help certain individual patients over others. This emerging area of science, which has been evolving rapidly over recent years, entails understanding the use of both personalised and precision medicine.
This webinar discusses examples of personalised and precision medicine, explains the role these tools play in treating autoimmune disease and discusses how incorporating them can improve patients’ responses to treatment.
Fast Facts from the Webinar
1. Precision and personalised medicine refer to different aspects of a person’s individualised treatment plan
Precision and personalised medicine take different sets of information into account in order to find the best treatment for an individual based on their unique characteristics and needs.
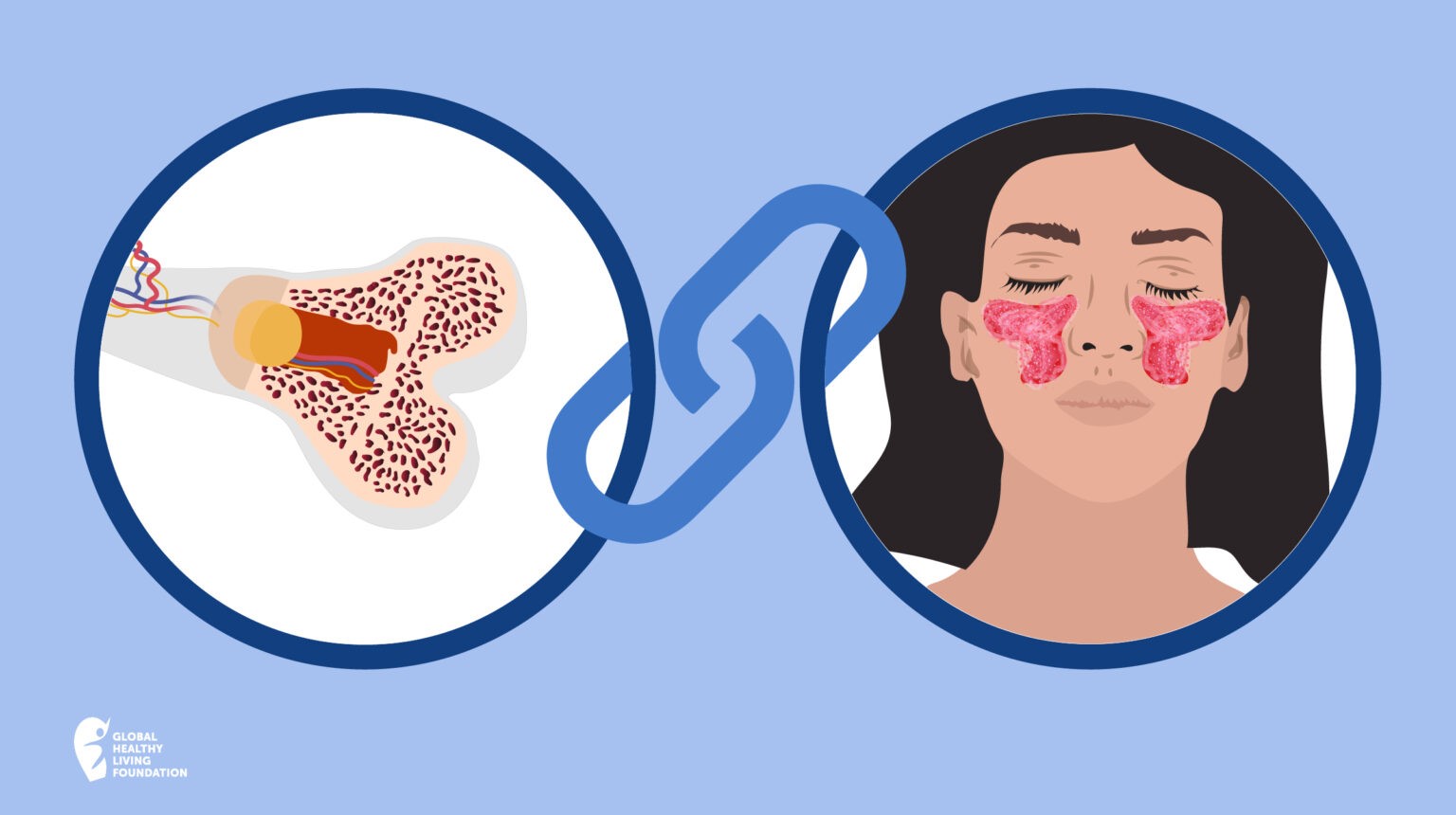
- Precision medicine takes into consideration things such as labs, hereditary information and individualised genetics.
- Personalised medicine refers to everything that you speak to your doctor about and may not be observed in lab tests. It may include things like speaking about depression, anxiety and sleep disturbances, as well as talking to your doctor about your preferences (such as a preference for taking a medication in a tablet form versus an infusion) and goals.
2. Precision medicine can help in the treatment and prevention of diseases
The goal of precision medicine is to make patients healthier by more quickly determining what kind of treatment and medication may best work for an individual.
The long-term aim of precision medicine is for patients to be able to take simple tests that can provide information about exactly what kind of medications work best for their specific disease. (For example, would a patient with RA be more likely to do well on one biologic versus another, based on the specific traits of their disease, their genetic makeup or personal history.) This would be ideal compared to what happens today, where usually the journey to find appropriate treatment often requires more of a trial and error process of going through various treatments first.
Precision medicine may also provide information about what treatment to start to prevent a disease from altering your life. Precision medicine aims to keep healthy patients even healthier by preventing diseases in the first place.
3. Precision medicine can work better for certain diseases than others
Precision medicine is more advanced in some diseases compared to others, but the hope is that all diseases will benefit from this science over time. This is already the case with a few types of cancer, such as lung cancer and breast cancer. As precision medicine advances through pharmacogenomics (using genetic testing to determine the best treatment for an individual), there is increased focus on developing and using different tests to identify the best treatment for each individual quicker.
The above are just a few takeaways from the one-hour event. Check out the video above, or head over to youtube.com/CreakyJoints to view the webinar in its entirety.
The Patient Perspective
Here’s what patient participants said they learned from this webinar:
- “We can look forward to medication therapy directed toward DNA/genetics.” — Dana M.
- “I learned the difference between personalised and precision care and how it can help doctors.” — Jed F.
About the Presenter
Daniel Hernandez, MD, Medical Advocacy Liaison for the Global Healthy Living Foundation (GHLF)
Daniel Hernandez, MD, graduated from medical school at the Universidad Autonoma de Guadalajara and is now based in New York City where he leads medical education and Hispanic outreach. He was joined by CreakyJoints patients and staff for a one-hour webinar to discuss this topic.
Keep Reading
- How Well Do You Know Your Medications? Are You at Risk of an Overdose?
- 5 Ways Your GP Can Help You Manage Your Chronic Illness
- Classifications of Spondyloarthritis and Why They Matter
This article has been adapted, with permission, from a corresponding article by CREAKYSTAFF on the CreakyJoints US website. Some text and information has been changed to suit our Australian audience.