The CreakyJoints Australia team recently had the privilege of attending the Australian Rheumatology Association (ARA) 2022 Annual Scientific Meeting. The event drew on international, regional and Australian speakers including physicians, researchers, scientists, clinicians, other health and industry professionals and rheumatology patients.
The three-day meeting was held as a hybrid event with satellite hubs across Australia and New Zealand. This gave those who were able, the opportunity to gather in person for the first time since the start of the pandemic. The online platform allowed those who could not travel to the hubs due to distance, mobility issues or health concerns about COVID-19 to actively participate. Our team participated in person in Sydney and virtually from Melbourne and Flinders Island (Tasmania).
Our goal was to attend as many sessions as possible, focusing on those related to consumer engagement, the latest prevention and treatment research, COVID-19 implications for rheumatology patients and paediatric rheumatology.
We were also very active on Twitter throughout the event using the hashtag #ARA22.
With so many informative sessions and posters on offer, it was hard for us to pick our favourites. Here are some we thought you’d like to know about.
COVID-19 session
Early treatment of COVID-19
Cassandra Calabrese is an Assistant Professor of Medicine at the Cleveland Clinic Lerner College of Medicine. In this session, Dr Calabrese outlined the optimal use of COVID-19 treatments in the early stage of symptoms. The earlier they are administered, the better.
There are several forms of COVID-19 antiviral therapies used in Australia. Clinicians use a combination of factors to decide the most appropriate antiviral to prescribe. These include:
- The age of the patient
- How long they have had COVID-19 symptoms
- The severity of their symptoms (for example, if they require oxygen)
- Their other health conditions
- The medications they currently take
Therefore, it is very important for all of us to have an up-to-date copy of our medical history and current medications (including supplements) easily accessible if we need to seek medical care for COVID-19.
(The NPS MedicineWise app is an ideal way to keep track of your medications, appointments, healthcare providers and more.)
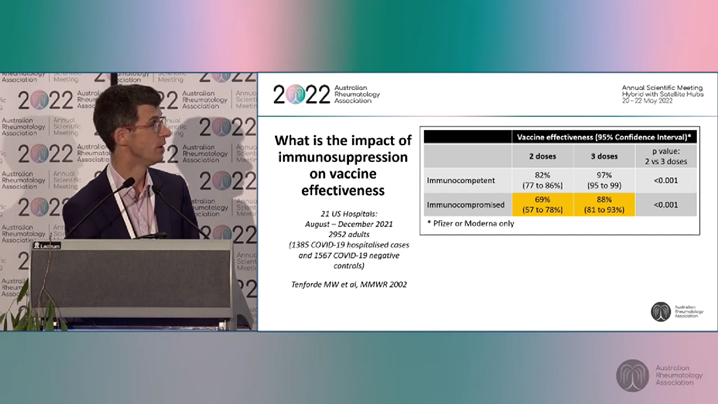
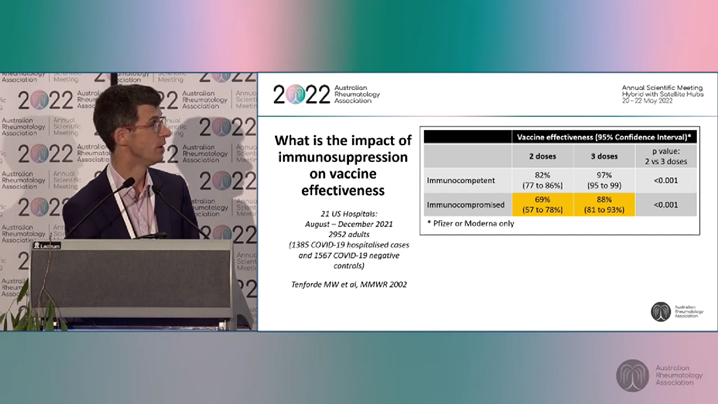
COVID-19 vaccine efficacy
Professor Chris Blyth is the Head of Infectious Diseases at Perth Children’s Hospital and a former co-chair of ATAGI. In this presentation, Professor Blyth discussed vaccine efficacy in immunosuppressed people. “Generally, COVID-19 vaccines work well against severe disease but less well against milder cases,” he said.
Professor Blyth added that waning vaccine effectiveness over time is especially noticeable in the elderly, the severely immunosuppressed and the very young. Pre-winter booster doses are currently recommended for the first two groups.
Relationship between COVID-19 and immunosuppression disease
Philip Robinson is an Associate Professor at the University of Queensland Faculty of Medicine and the chair of the steering committee for the COVID-19 Global Rheumatology Alliance. He stressed that the biggest risk for people with rheumatic disease who get COVID-19 is not their condition or immunosuppressive treatments but rather the comorbidities they have. Age, ethnicity and obesity also contributing factors.
All three speakers stressed rheumatologists can do more to educate patients about COVID-19 management by sharing information on:
- Recognising the signs and symptoms of COVID-19 and knowing when to seek medical care.
- Accessing, understanding and administering home testing.
- Knowing who to contact if they have suspected/documented COVID-19 or are at high-risk of contracting it.
- Understanding the urgency and advantages of early treatment and prevention (such as taking antivirals within five days of the onset of symptoms).
- Knowing how to find and access all the resources and services available to them.
(See the GHLF Australia COVID-19 self-care guide: Essential pre-planning information for people with chronic conditions for more information.)
Consumers in Research session
Consumer representative and advocate, Ben Horgan, from the Western Australian Health Translation Network’s Consumer and Community Involvement Program spoke of the increasing role of health consumers in health research.
Our lived experience and perspectives are increasingly being seen as a key component in shaping decisions about research priorities, policy and practice. This allows for greater transparency, openness and accountability leading to research which is more relevant and impactful to the community.
“Consumer and community involvement is about research being carried out with or by consumers and community members rather than to, about or for them,” he said. “Consumers look at things in a different way because it means different things to them … It is going to become the norm for consumer involvement to be a key requirement for research funding.”
Suzie Edward May is one of the experienced consumer advocates involved in the design and development of the Australian Living Guideline for the Pharmacological Management of Inflammatory Arthritis.
This living guideline is being produced by the Australia and New Zealand Musculoskeletal (ANZMUSC) Clinical Trials Network, the Australian Rheumatology Association (ARA) and Cochrane Musculoskeletal, as part of the Targeted Therapies Alliance, led by NPS MedicineWise.
The aim of this living guideline is to present the best available, current scientific evidence for pharmacological management of the most common forms of inflammatory arthritis (IA), namely rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis. It is intended for use by medical practitioners who treat IA. However, the guideline will also be relevant to GPs and others involved in the care of patients with IA and also for pharmacists and consumers.
Living guidelines are:
- A move away from the traditional method of guideline development
- A continual evidence search followed by rapid updates to recommendations
- A tool to guide medical practitioners in their care, treatment and management based on up-to-date evidence.
- A tool for communication between practitioners and patients to guide shared decision making.
Recommendations are intended as guides to courses of action subject to clinical judgement and patient preferences. This living guideline was first published in 2020 and is updated every three months.
Annie MacPherson is the president of Ankylosing Spondylitis Victoria and the chair of the ANZMUSC Consumer Advisory Group. She outlined the processes and challenges involved with establishing this group in 2016.
At that time, many researchers did not fully understand the role consumers could play in the design, planning and reviews of clinical trials. One of their early tasks was to help re-write their team’s research guidelines to make them more consumer-focused. Today, the group is an essential and growing part of the ANZMUSC team.
The three advocates highlighted the growing need for health consumers to get involved in all levels of research. They stressed that lived experience is an essential factor and that a greater emphasis should be put on training consumers in health literacy and advocacy.
Inducing Remission in Immune-Mediated Inflammatory Disease
Evolution of the treatment of inflammatory diseases
Georg Schett is a Professor of Internal Medicine and Head of the Department of Rheumatology and Immunology at Universitätsklinikum Erlangen, Friedrich-Alexander University Erlangen-Nürnberg in Germany.
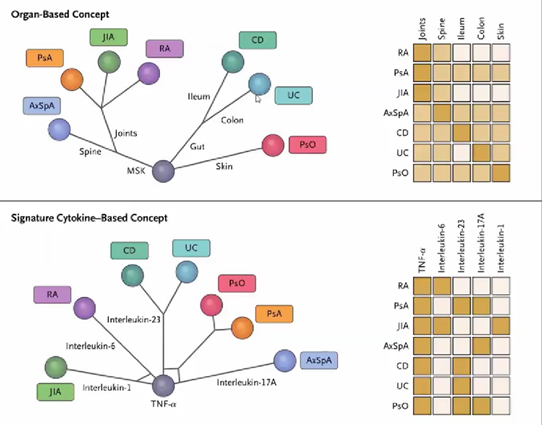
Professor Schett outlined how, until the introduction of monoclonal antibodies to target specific immune system cells in the 1980s, groups of diseases were treated based on similarities in organ involvement. For example, psoriasis and leprosy were treated in similar ways as they look very similar but the treatment outcomes were unreliable and varied.
We now know that regulating cytokines (types of protein cells that are crucial in controlling the growth and activity of specific immune system and blood cells) can significantly reduce disease activity in many patients with autoimmune inflammatory diseases. Diseases that look quite different and have different organs involved can have similar cytokine involvement. Therefore, they can be treated in similar ways.
The discovery that an entire inflammatory disease (like rheumatoid arthritis) could be based on a single cytokine like TNF was revolutionary. The whole network of inflammation can break down if you target the signature cytokine in a disease. For example, in rheumatoid arthritis it is TNF and interleukin 6 but it is different in inflammatory bowel disease (ulcerative colitis and Crohn’s disease) and psoriasis. Therefore, targeting the treatment to the type of cytokine activity reaps the most benefits.
The diagram below shows how the diseases axial spondyloarthritis (AxSpA), psoriatic arthritis (PsA), juvenile idiopathic arthritis (JIA), rheumatoid arthritis (RA), Crohn’s disease (CD), ulcerative colitis (UC) and psoriasis (PsO) have very different organ and cytokine involvement.
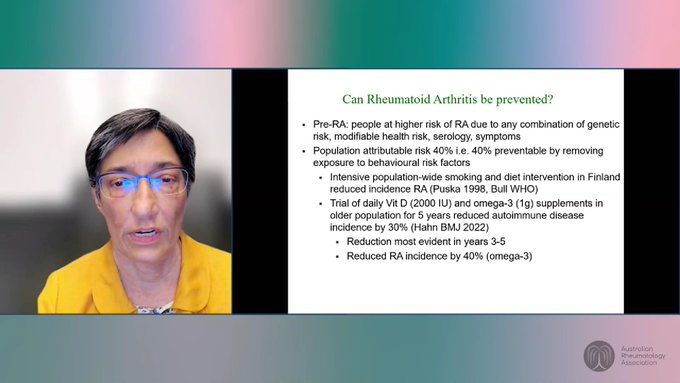
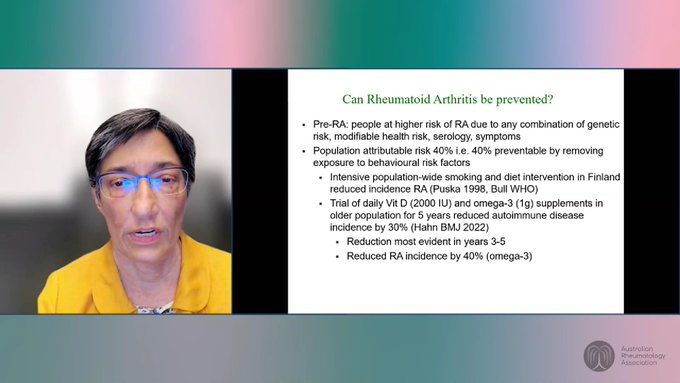
Can rheumatoid arthritis be prevented?
Ranjeny Thomas is a Professor of Rheumatology at University of Queensland, Translational Research Institute and member of the Order of Australia. She shared that those in general population who test positive for ACPA (anti-citrullinated protein antibody) have a 9 per cent chance of progression to RA. First degree relatives of people with RA have a three to nine-fold risk of progression to disease. Rheumatoid arthritis also affects more women than men.
Symptom indicators include:
- Symmetrical joint involvement
- Prolonged morning stiffness
- High tender or swollen joint counts
- High levels of C-reactive protein (CRP) in the blood (indicating inflammation)
- Tenosynovitis in the hands
Studies show that 40 per cent of rheumatoid arthritis cases are potentially preventable by identifying pre-RA signs and removing exposure to behavioural risk factors. Protections that can help reduce disease progression include:
- Ceasing smoking
- Anti-inflammatory diet
- Vitamin D and omega 3
- Exercise
- Reduce alcohol and soft drinks
- Pregnancy and breastfeeding promote regulation for as long as they last
Professor Thomas noted that simply losing weight (such as through weight-loss surgery) does not change the risk of disease progression. Weight loss must be combined with a sustained healthy diet.
In the pre-RA period, as people get closer to onset of RA, Professor Thomas and other rheumatologists are increasingly likely to intervene with treatments. These may initially be lifestyle changes only and are always based on shared decisions with patients.
The A3BC Centre of Research Excellence for Better Outcomes in Inflammatory Arthritis is currently rolling out research centres across Australia for people at risk of developing inflammatory arthritis.
The aims of this project include collecting Australian genetic biosamples, data on risk factors for disease progression and trials of lifestyle and therapeutic interventions in the pre-RA stage.
They are looking for people at risk to get involved and more information will be on the A3BC website soon. In the meantime, interested people can contact the project team via info@a3bc.org.au.
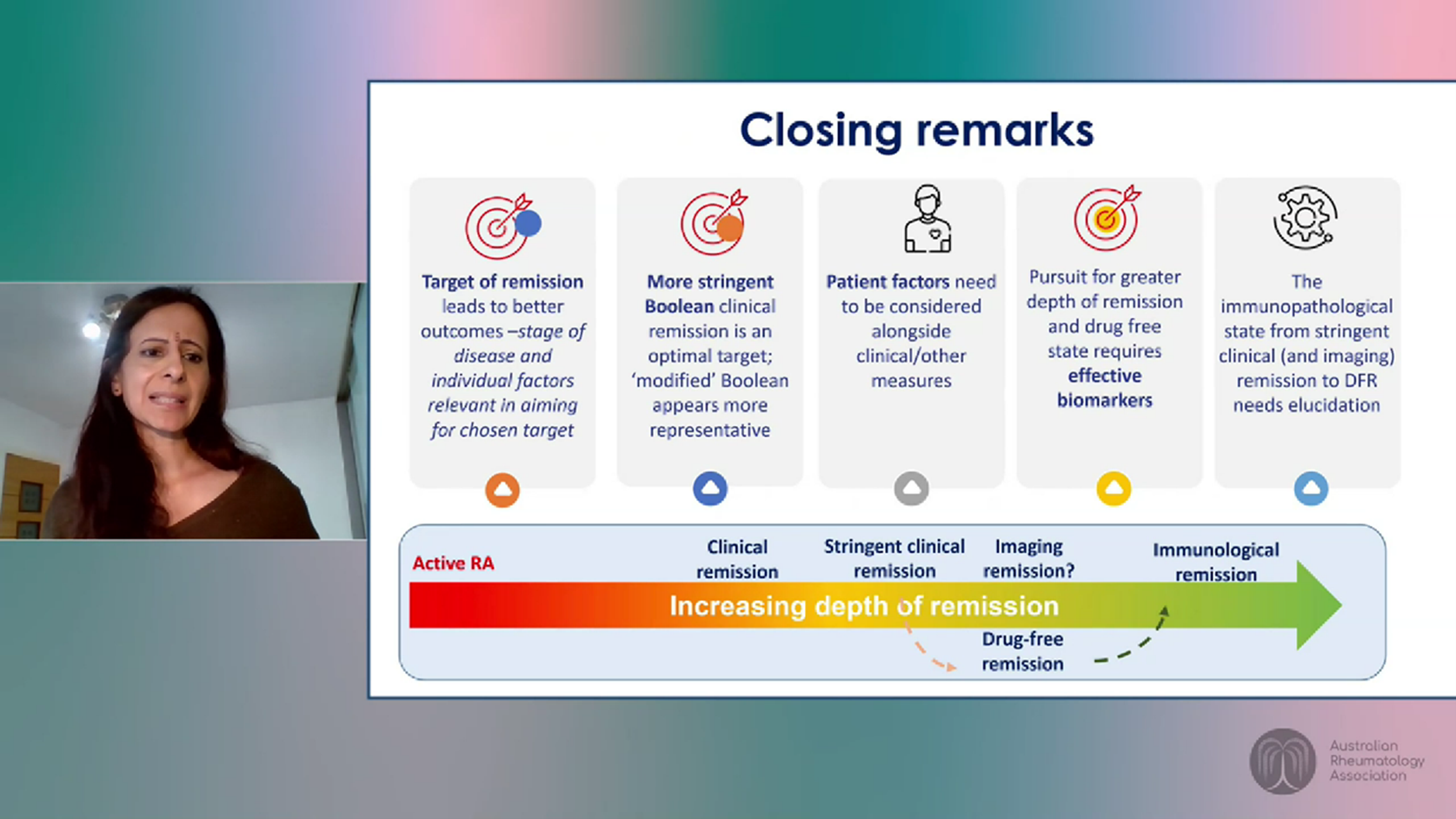
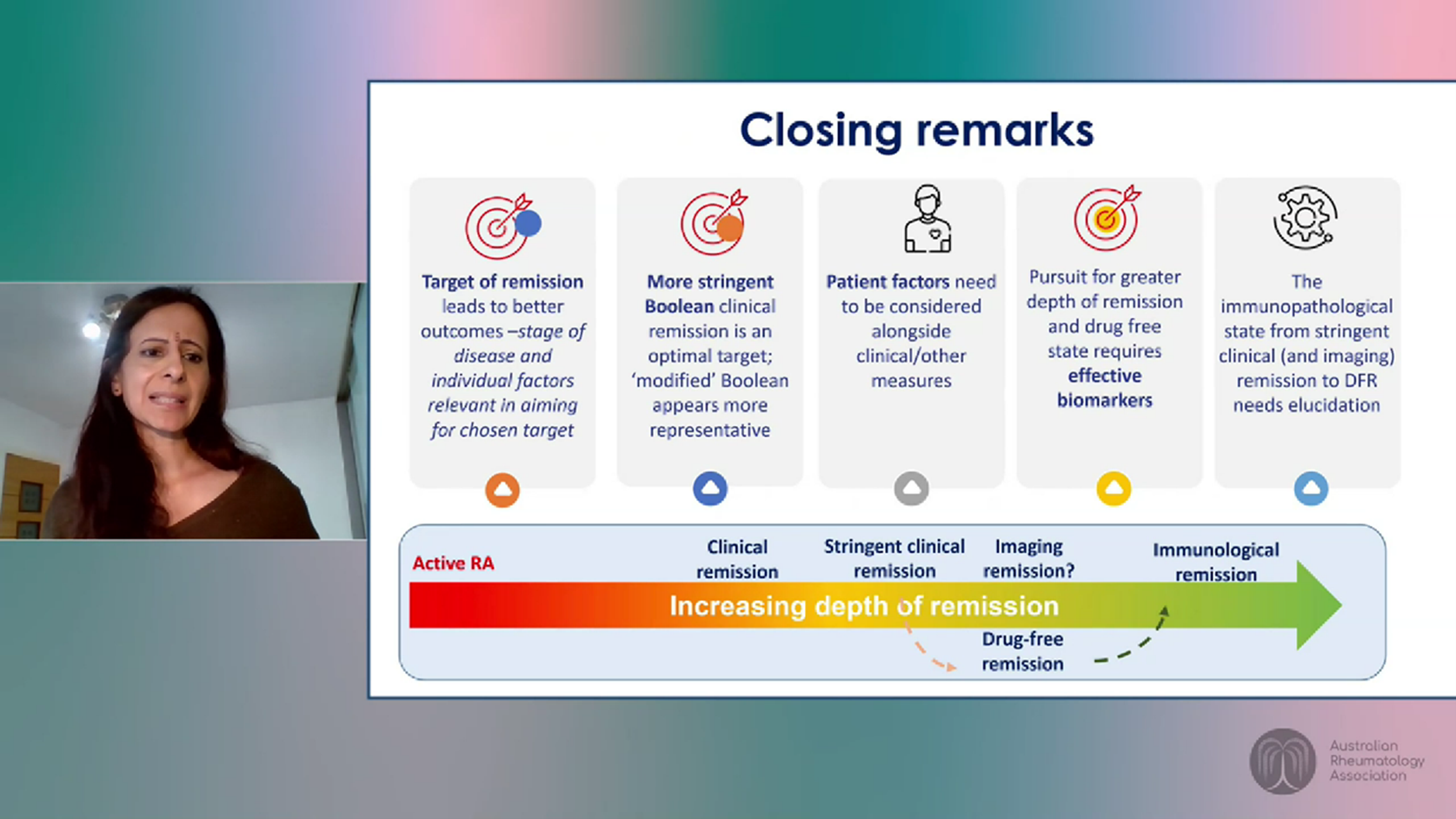
Challenges of remission as a treatment target.
Inflammatory diseases such as rheumatoid arthritis currently have no proven cure. Remission without scientifically-proven treatment is extremely rare, however, levels of treatment-induced remission are possible in many cases.
We know that achieving remission improves outcomes and reduces patient burden beyond the signs and symptoms of the disease. For example, it decreases the risk of other conditions such as cancer, osteoporosis, cardiovascular disease and infections. It also reduces the likelihood of poor psychological and socioeconomic outcomes.
Maya Buch is a Professor of Rheumatology at the University of Manchester and NIHR Manchester Biomedical Research Centre. She noted that one of the key challenges of aiming for remission in inflammatory diseases is that there is no universal consensus on what remission looks like.
The main types of remission include:
- Clinical remission – the absence or low-level of disease activity measured by scores such as the DAS 28, CDAI and Boolean criteria.
- Imaging/serological remission – clinical remission plus no signs of disease markers using standard ultrasounds, MRIs or blood tests.
- Immunological remission – imaging/serological remission plus negative test results for rheumatoid factor and ACPA biomarkers.
Clinical remission is assessed by scoring systems that have pros and cons in terms of feasibility as well as interpretation. However, results do not necessarily translate into disease control. Comorbidities such as fibromyalgia can also affect results.
The type of intervention can also influence the ability to achieve remission. For example, drugs that target interleukin 6 directly relate to CRP production can skew DAS28 scoring and therefore, achievement of remission rates. The Boolean remission criteria is much more stringent but may be very difficult to achieve.
Professor Buch noted there is often a disconnect between what clinicians and their patients define as remission. It is important for both to have in depth discussions to agree on their desired objectives. Factors that patients rate as essential to characterise remission include reduced or absent pain, greater independence and less (or no) fatigue.
Some patients may have long periods of being symptom-free but they may not be technically in remission. For some, this can be more important than achieving a technical definition.
There is currently active debate about whether clinicians should be tapering medications and aiming for drug-free remission but more research needs to be done before we can draw strong conclusions. In the meantime, many clinicians are making decisions with select patients based on their circumstances and preferences.
ePosters
There were 103 research posters presented via the ARA 2022 virtual platform. CreakyJoints Australia team members had direct connections with two of them.
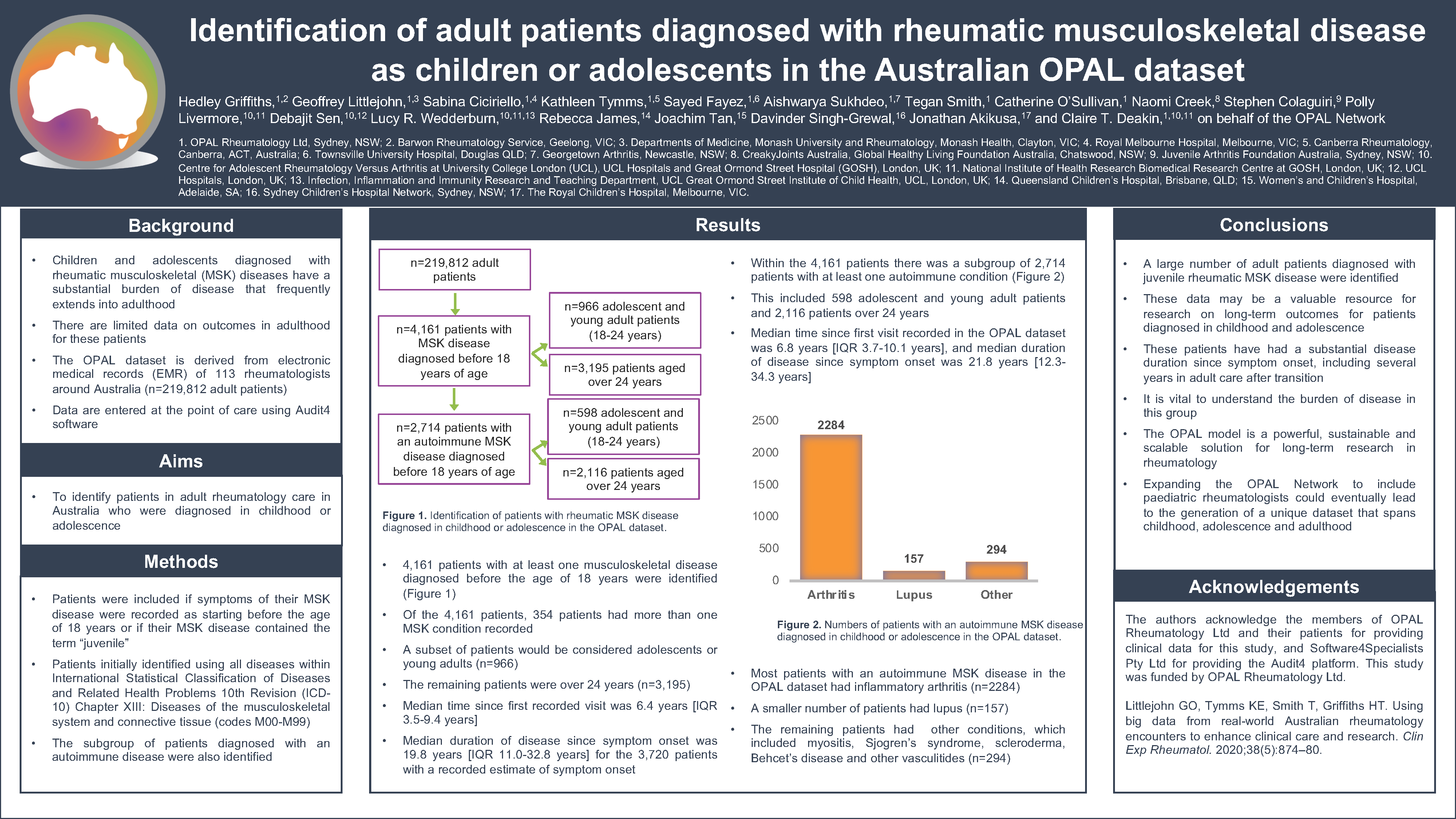
Poster 17: Identification of adult patients diagnosed with rheumatic musculoskeletal disease as children or adolescents in the Australian OPAL dataset
Poster contributors
Hedley Griffiths, Geoffrey Littlejohn, Sabina Ciciriello, Kathleen Tymms, Sayed Fayez, Aishwarya Sukhdeo, Tegan Smith, Catherine O’Sullivan, Naomi Creek1, Stephen Colaguiri, Polly Livermore, Debajit Sen, Lucy R. Wedderburn, Rebecca James, Joachim Tan, Davinder Singh-Grewal, Jonathan Akikusa, and Claire T Deakin on behalf of the OPAL Network.
1 Naomi Creek is the CreakyJoints Australia National Coordinator
Poster summary
Children and adolescents diagnosed with rheumatic musculoskeletal (MSK) diseases have a substantial burden of disease that frequently extends into adulthood. However, there is limited data on outcomes in adulthood for these patients.
The aim of the research was to identify patients in adult rheumatology care in Australia who were diagnosed in childhood or adolescence. The research was conducted using the OPAL Network dataset, derived from electronic medical records of 113 rheumatologists around Australia using deidentified patient data.
The research found a large number of adult patients who had been diagnosed with juvenile rheumatic MSK disease. These patients have had a substantial disease duration since the inset of their symptoms, including several years in adult care after transition. Therefore, it is vital to understand the burden of disease in this group.
Information derived from these adults may be a valuable resource for research on long-term outcomes for patients diagnosed in childhood and adolescence.
The OPAL model is a powerful, sustainable and scalable solution for long-term research in rheumatology. Expanding the OPAL network to include paediatric rheumatologists could eventually lead to the generation of a unique dataset that spans childhood, adolescence and adulthood.
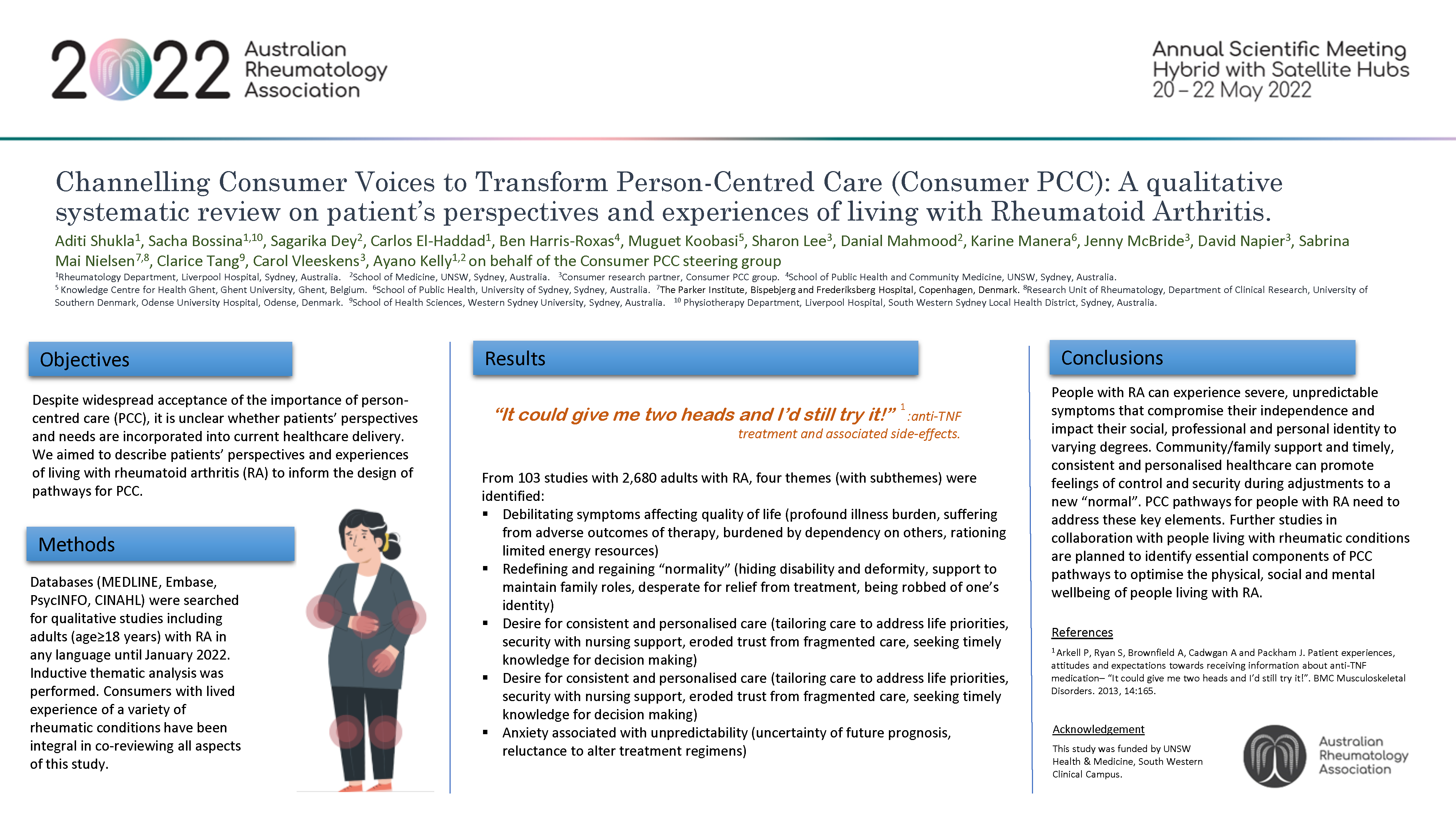
Poster 89: Channelling Consumer Voices to Transform Person-Centred Care (Consumer PCC): A qualitative systematic review on patient’s perspectives and experiences of living with Rheumatoid Arthritis
Poster contributors
Aditi Shukla, Sacha Bossina1, Sagarika Dey, Carlos El-Haddad, Ben Harris-Roxas, MuguetKoobasi, Sharon Lee, Danial Mahmood, Karine Manera, Jenny McBride, David Napier, Sabrina Mai Nielsen, Clarice Tang, Carol Vleeskens, Ayano Kelly on behalf of the Maridulu Budyari Gumal/SPHERE Musculoskeletal Clinal Academic Group – Consumer Person-Centred Care Study steering group.
CreakyJoints Australia Editor, Rosemary Ainley, has since become a consumer representative in this steering group.
Poster summary
Despite widespread acceptance of the importance of person-centred care (PCC), it is unclear whether patients’ perspectives and needs are incorporated into current healthcare delivery. This qualitative systematic review aimed to describe patients’ perspectives and experiences of living with rheumatoid arthritis (RA) to inform the design of pathways for PCC.
The review found people with RA can experience severe, unpredictable symptoms that compromise their independence and impact their social, professional and personal identity to varying degrees. Community/family support and timely, consistent and personalised healthcare can promote feelings of control and security during adjustments to a new “normal”. PCC pathways for people with RA need to address these key elements.
Further studies in collaboration with people living with rheumatic conditions are planned to identify essential components of PCC pathways to optimise the physical, social and mental wellbeing of people living with RA.