

Anyone with inflammatory arthritis or a related musculoskeletal disease has wrestled with fatigue. Fatigue is not just being very tired, like how you might feel after staying up too late. Fatigue is a physical issue: It’s a chronic weakness and lack of energy that prevents you from doing your usual daily activities. “I used to go-go-go for 10- or 12-hour days,” Veronica W told us (on the CreakyJoints US Facebook page). “Now I have to take a nap after just having a shower. The fatigue is unbelievable.”
Fatigue is a controversial subject among chronic illness patients because it’s a debilitating — yet often invisible — symptom. It can be difficult for family, friends and coworkers without chronic illness to understand the impact that fatigue has on quality of life and your ability to get through the day, work and engage in errands and social activities.
It’s important to study fatigue and its impact on patients so doctors and researchers can better understand how to treat it, and for loved ones to provide empathy and support to patients living with the burdens of daily fatigue.
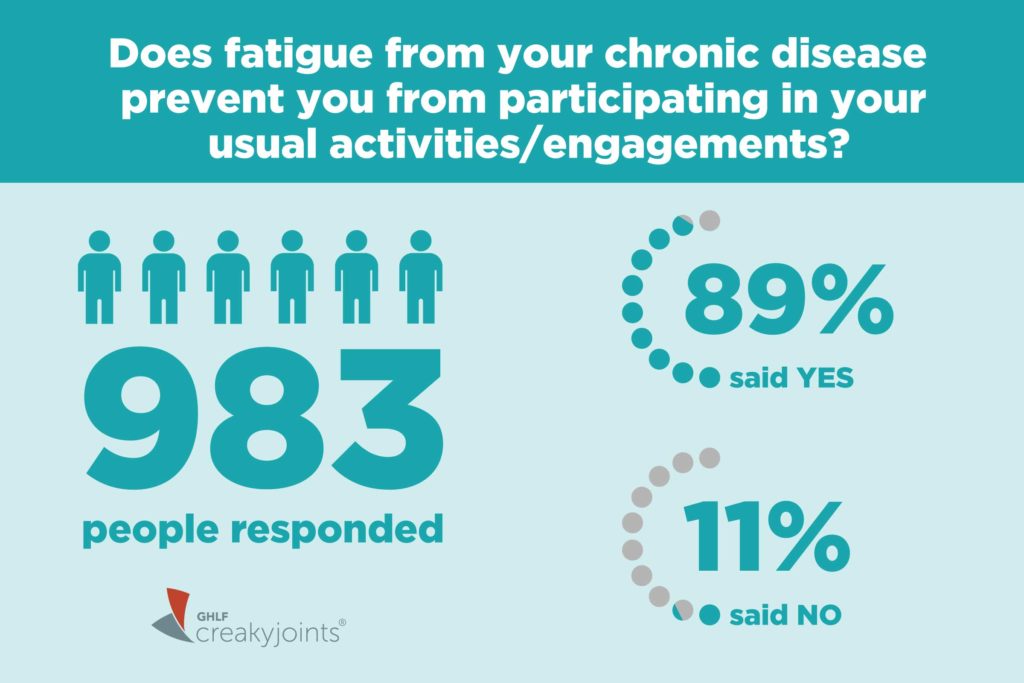
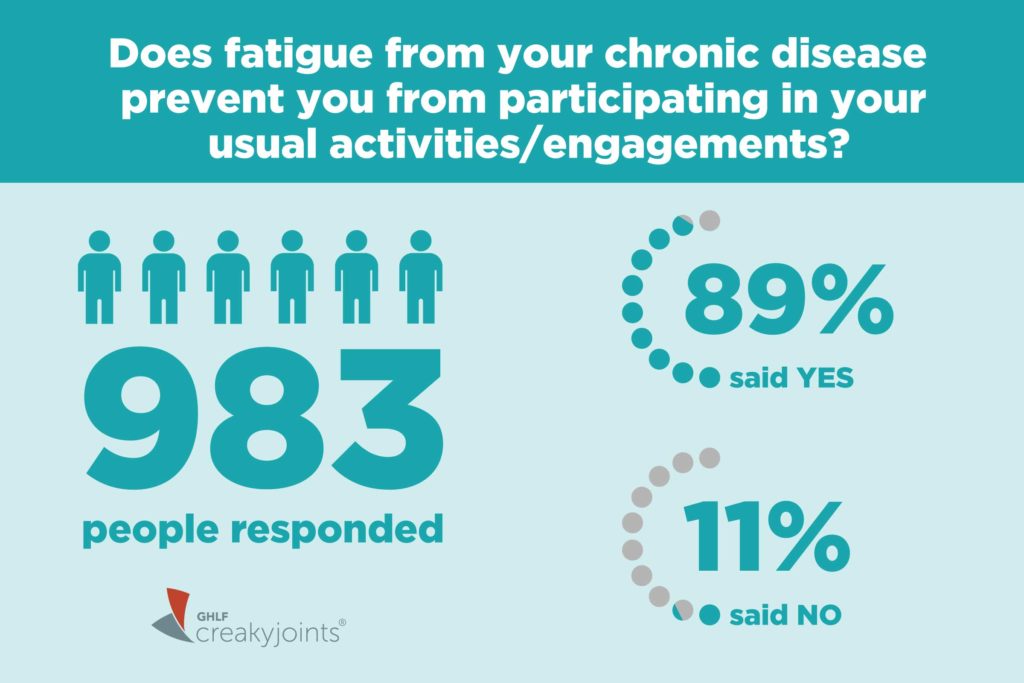
We wanted to understand how our community felt about this issue, so we asked our members in a recent Community Poll: Does fatigue from your chronic disease prevent you from participating in your usual activities/engagements?
Nearly nine in 10 of 983 respondents said it does.
Arthritis patients may experience fatigue because of inflammation that stresses the body. Chronic pain is also a big factor, since it often interferes with sleep — and lack of sleep, in turn, can worsen pain. Medications you take to treat your arthritis symptoms play a role too. While disease-modifying antirheumatic drugs (DMARDs) like biologics can ultimately reduce inflammation and pain, many patients report that these medications contribute to symptoms of fatigue, especially on the day of and the days following their dose.
If you can relate to our poll respondents and feel that your fatigue is preventing you from participating in your usual activities, know that 1) you’re not alone; and 2) there are things you can do — both with your doctor and through lifestyle adjustments — to help manage and reduce fatigue.
One important first step is to start tracking your fatigue. (Try using an app or notebook for this.) When you take note of when your fatigue feels worse, you can be more informed to talk to your doctor about how to manage it better. You might observe that your fatigue feels worse on days when pain is keeping you awake at night or on days you take your arthritis medication, for example.
Unfortunately, there is no quick remedy to eliminate chronic fatigue. Patients should work with their doctor to tailor options to their unique needs. More often than not, suggestions for dealing with fatigue fall into one of these categories:
- Make lifestyle changes (sleep, diet, exercise, self-care)
- Adjust medications by dose reduction, changing the class of medication or the timing of when you take medication (many patients prefer taking weekly medications right before the weekend so they can have time to rest)
- Find and treat underlying medical issues that may be contributing to fatigue
- Seek therapy and emotional help through support groups
Patients’ Tips for Coping With Fatigue
We asked our CreakyJoints US Facebook community for their advice on how they deal with fatigue. Here are some of their tips:
Stick to a schedule: “When fatigue hits, there’s not much I can do but give in and rest,” says Mary Y. The one thing that somewhat helps lessen the frequency of fatigue is keeping a regular schedule that includes enough hours for rest and getting a small amount of gentle exercise.
Give yourself mini rests: Sophie says that her chronic fatigue syndrome nurse taught her that “I need to take breaks throughout the day to recharge. It just needs to be five or 10 minutes, but during that time, you don’t do anything. No electronics, no food, no reading: just sit and recharge. It’s actually one of the hardest things I’ve had to learn to do, but it works. It isn’t a cure but it makes it easier to get through the day or at least fend off a major crash if there’s something that I can’t put off.”
Make a divide between work and home: When Alison P gets home from work, she feels like she’s hit a brick wall. Napping on the sofa right when she gets home helps her get her energy levels back. Plus: “I relax in a bath every night. I can’t fight this; I just learn what I can do and adjust,” she adds.
Take advantage of a flexible work schedule: Roz D, who works from home, learned to arrange her work day to maximize her energy levels. She would work first thing in the morning, nap in the early afternoon, and work again in the late afternoon.
“If I’m at home and not working, a short nap helps me,” echoes Ranay C. “If working, taking a short power nap during a lunch break works to help alleviate the fatigue. Moving is a must if a nap isn’t possible.”
Know when napping isn’t right for you: While many patients swear by napping to help manage fatigue, for some people napping could actually make the problem worse. “I won’t rest or nap during the day,” says Tracey E. “I don’t sleep at night and don’t want to make this even worse.” When she feels fatigue, she tries to combat it by moving around. “[Fatigue] just comes over me. I can feel my eyes going but feel powerless to stop it. That’s why I have to move,” she says.
Take alone time: Fatigue can be a recipe for grumpiness, so feel free to opt out of plans and events in the spirit of your self-care. “I do allow myself to not ‘people’ if I am too tired. Alone time does wonders for me,” says Jenny K.


Give yourself permission to hibernate: “For me it’s a home day — or a few — in PJs and doing very little,” says Sue M. However, it’s important to watch for signs of depression and loneliness. Finding a circle of loved ones and friends you can reach out to during bouts of bad fatigue — even if it’s just over text messages or social media — can help you avoid feeling totally disconnected from the rest of the world.
Rest between tasks: “When I get fatigued, I go to my room and rest for a little bit to regain strength before I go back to do things around the house like cooking and cleaning,” says J Diaz Y.
Eat energising snacks: Helena B acknowledges that “sometimes the fatigue is so strong I can barely lift my arms or keep my eyes open.” She finds that “having some fruit and some electrolytes” helps, as does lying down for a short snooze or doing gentle stretching.
Walk for an energy boost: In addition to taking vitamins and eating fruit and keto-friendly desserts at work, Andrea H says she walks whenever possible.
Let yourself get more sleep at night: “I must have 10 to 12 hours of sleep every night,” says Nana C. She also says she has to pace herself for any shopping or cleaning and try to avoid “upsets or stressors from my adult kids, friends or neighbors.”
Be careful with your caffeine timing: Drinking caffeine too late in the day can interfere with your ability to sleep well at night, creating a vicious cycle of insomnia that factors in to daytime fatigue. “I have a system where I drink no caffeinated beverages after 12 noon,” says Joyce F. “Before I go to bed I shower, which prepares my mind for sleep. I also follow an anti-inflammatory diet which seems to help.”
Keep Reading
- How the Spoon Theory Helps Me Explain the Fatigue of Chronic Illness
- 5 Ways Your GP Can Help You Manage Your Chronic Illness
- Practical Tips for Cooking With Arthritis: Making Kitchen Tasks Easier
- Chronic Pain and Sleep
- 5 tips for getting the most out of a peer support group
This article has been adapted, with permission, from a corresponding article by Lauren Gelman on the CreakyJoints US website. Some content may have been changed to suit our Australian audience.




